
English Reading Materials Chapter 33:Agents That Affect Bone Mineral Homeostasis I.BASIC PHARMACOLOGY INTRODUCTION Calcium and phosphate,the major mineral constituents of bone,are also two of the most important minerals for general cellular function.Accordingly,the body has evolved a complex set of mechanisms by which calcium and phosphate homeostasis are carefully maintained(Figure 1).Approximately 98%of the 1-2 kg of calcium and 85%of the 1 kg of phosphorus in the human adult are found in bone,the principal reservoir for these minerals.These functions are dynamic,with constant remodeling of bone and ready exchange of bone mineral with that in the extracellular fluid.Bone also serves as the principal structural support for the body and provides the space for hematopoiesis.Thus,abnormalities in bone mineral homeostasis can lead not only to a wide variety of cellular dysfunctions (eg,tetany,coma,muscle weakness)but also to disturbances in structural support of the body (eg,osteoporosis with fractures)and loss of hematopoietic capacity (eg,infantile osteopetrosis). Calcium and phosphate enter the body from the intestine.The average American diet provides 600-1000 mg of calcium per day,of which approximately 100-250 mg is absorbed.This figure represents net absorption,because both absorption(principally in the duodenum and upper jejunum)and secretion(principally in the ileum)occur. The amount of phosphorus in the American diet is about the same as that of calcium. However,the efficiency of absorption(principally in the jejunum)is greater,ranging from 70%to 90%,depending on intake.In the steady state,renal excretion of calcium and phosphate balances intestinal absorption.In general,over 98%of filtered calcium and 85%of filtered phosphate is reabsorbed by the kidney.The movement of calcium and phosphate across the intestinal and renal epithelia is closely regulated.Intrinsic disease of the intestine (eg,nontropical sprue)or kidney (eg,chronic renal failure) disrupts bone mineral homeostasis. Two hormones serve as the principal regulators of calcium and phosphate homeostasis: the peptide parathyroid hormone(PTH)and the steroid vitamin D(Figure 2).Vitamin D is a prohormone rather than a true hormone,because it must be further metabolized to gain biologic activity.PTH stimulates the production of the active metabolite of vitamin D,1,25(OH)2D.1,25(OH)2D,on the other hand,suppresses the production of PTH.1,25(OH)2D stimulates the intestinal absorption of calcium and phosphate. 1,25(OH)2D and PTH promote both bone formation and resorption in part by stimulating the proliferation and differentiation of osteoblasts and osteoclasts.Both PTH and 1,25(OH)2D enhance renal retention of calcium,but PTH promotes renal
English Reading Materials Chapter 33: Agents That Affect Bone Mineral Homeostasis I. BASIC PHARMACOLOGY INTRODUCTION Calcium and phosphate, the major mineral constituents of bone, are also two of the most important minerals for general cellular function. Accordingly, the body has evolved a complex set of mechanisms by which calcium and phosphate homeostasis are carefully maintained (Figure 1). Approximately 98% of the 1-2 kg of calcium and 85% of the 1 kg of phosphorus in the human adult are found in bone, the principal reservoir for these minerals. These functions are dynamic, with constant remodeling of bone and ready exchange of bone mineral with that in the extracellular fluid. Bone also serves as the principal structural support for the body and provides the space for hematopoiesis. Thus, abnormalities in bone mineral homeostasis can lead not only to a wide variety of cellular dysfunctions (eg, tetany, coma, muscle weakness) but also to disturbances in structural support of the body (eg, osteoporosis with fractures) and loss of hematopoietic capacity (eg, infantile osteopetrosis). Calcium and phosphate enter the body from the intestine. The average American diet provides 600-1000 mg of calcium per day, of which approximately 100-250 mg is absorbed. This figure represents net absorption, because both absorption (principally in the duodenum and upper jejunum) and secretion (principally in the ileum) occur. The amount of phosphorus in the American diet is about the same as that of calcium. However, the efficiency of absorption (principally in the jejunum) is greater, ranging from 70% to 90%, depending on intake. In the steady state, renal excretion of calcium and phosphate balances intestinal absorption. In general, over 98% of filtered calcium and 85% of filtered phosphate is reabsorbed by the kidney. The movement of calcium and phosphate across the intestinal and renal epithelia is closely regulated. Intrinsic disease of the intestine (eg, nontropical sprue) or kidney (eg, chronic renal failure) disrupts bone mineral homeostasis. Two hormones serve as the principal regulators of calcium and phosphate homeostasis: the peptide parathyroid hormone (PTH) and the steroid vitamin D (Figure 2). Vitamin D is a prohormone rather than a true hormone, because it must be further metabolized to gain biologic activity. PTH stimulates the production of the active metabolite of vitamin D, 1,25(OH)2D. 1,25(OH)2D, on the other hand, suppresses the production of PTH. 1,25(OH)2D stimulates the intestinal absorption of calcium and phosphate. 1,25(OH)2D and PTH promote both bone formation and resorption in part by stimulating the proliferation and differentiation of osteoblasts and osteoclasts. Both PTH and 1,25(OH)2D enhance renal retention of calcium, but PTH promotes renal
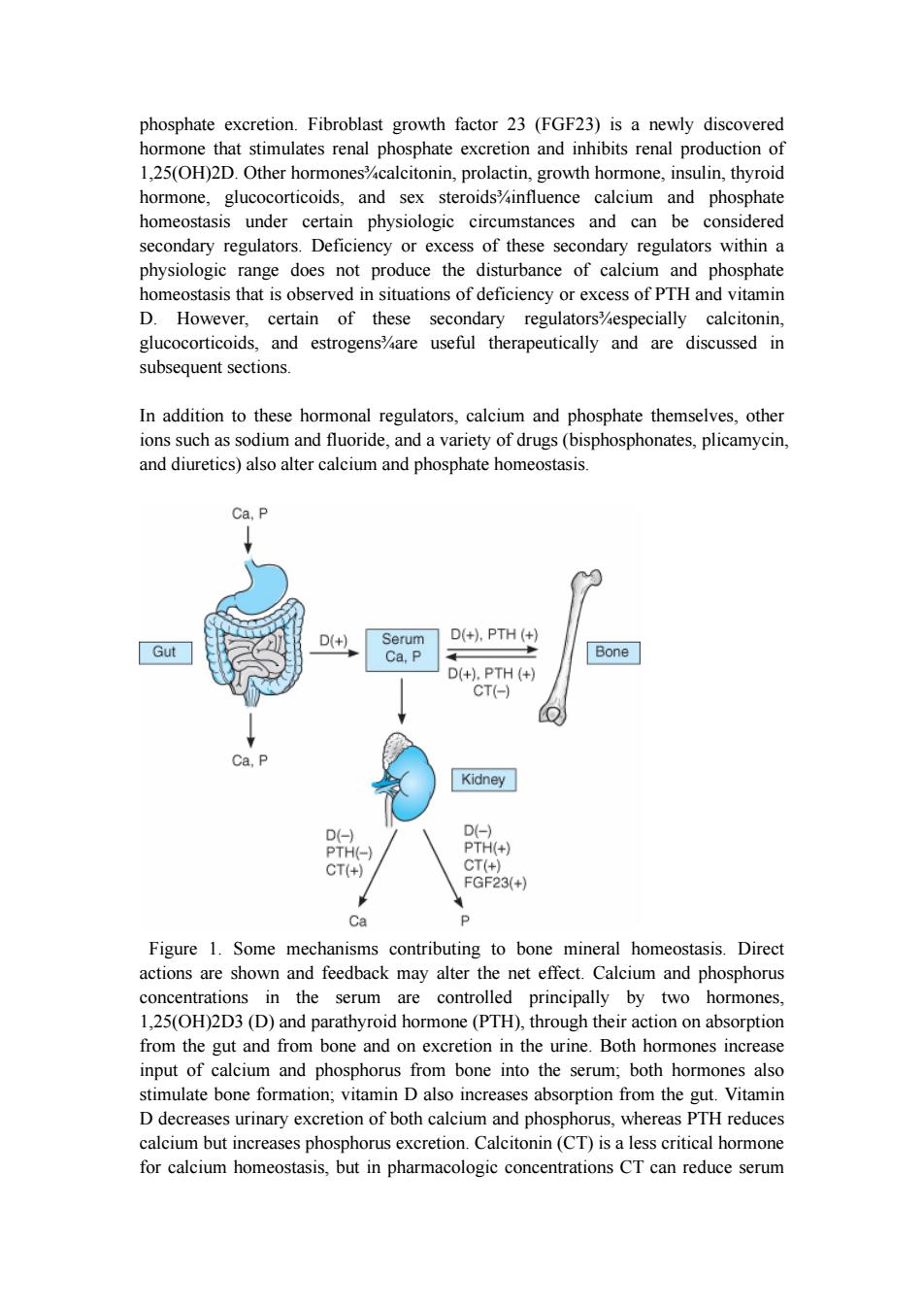
phosphate excretion.Fibroblast growth factor 23(FGF23)is a newly discovered hormone that stimulates renal phosphate excretion and inhibits renal production of 1,25(OH)2D.Other hormones%calcitonin,prolactin,growth hormone,insulin,thyroid hormone,glucocorticoids,and sex steroidsinfluence calcium and phosphate homeostasis under certain physiologic circumstances and can be considered secondary regulators.Deficiency or excess of these secondary regulators within a physiologic range does not produce the disturbance of calcium and phosphate homeostasis that is observed in situations of deficiency or excess of PTH and vitamin D.However,certain of these secondary regulators%especially calcitonin, glucocorticoids,and estrogens%are useful therapeutically and are discussed in subsequent sections. In addition to these hormonal regulators,calcium and phosphate themselves,other ions such as sodium and fluoride,and a variety of drugs(bisphosphonates,plicamycin, and diuretics)also alter calcium and phosphate homeostasis. Ca,P D(+) Serum D(+),PTH(+) Gut Ca,P Bone D(+),PTH(+) CT(-) Ca,P Kidney D(-) D(-) PTH(-) PTH(+) CT(+) CT(+) FGF23(+) Ca P Figure 1.Some mechanisms contributing to bone mineral homeostasis.Direct actions are shown and feedback may alter the net effect.Calcium and phosphorus concentrations in the serum are controlled principally by two hormones, 1,25(OH)2D3(D)and parathyroid hormone(PTH),through their action on absorption from the gut and from bone and on excretion in the urine.Both hormones increase input of calcium and phosphorus from bone into the serum;both hormones also stimulate bone formation;vitamin D also increases absorption from the gut.Vitamin D decreases urinary excretion of both calcium and phosphorus,whereas PTH reduces calcium but increases phosphorus excretion.Calcitonin(CT)is a less critical hormone for calcium homeostasis,but in pharmacologic concentrations CT can reduce serum
phosphate excretion. Fibroblast growth factor 23 (FGF23) is a newly discovered hormone that stimulates renal phosphate excretion and inhibits renal production of 1,25(OH)2D. Other hormones¾calcitonin, prolactin, growth hormone, insulin, thyroid hormone, glucocorticoids, and sex steroids¾influence calcium and phosphate homeostasis under certain physiologic circumstances and can be considered secondary regulators. Deficiency or excess of these secondary regulators within a physiologic range does not produce the disturbance of calcium and phosphate homeostasis that is observed in situations of deficiency or excess of PTH and vitamin D. However, certain of these secondary regulators¾especially calcitonin, glucocorticoids, and estrogens¾are useful therapeutically and are discussed in subsequent sections. In addition to these hormonal regulators, calcium and phosphate themselves, other ions such as sodium and fluoride, and a variety of drugs (bisphosphonates, plicamycin, and diuretics) also alter calcium and phosphate homeostasis. Figure 1. Some mechanisms contributing to bone mineral homeostasis. Direct actions are shown and feedback may alter the net effect. Calcium and phosphorus concentrations in the serum are controlled principally by two hormones, 1,25(OH)2D3 (D) and parathyroid hormone (PTH), through their action on absorption from the gut and from bone and on excretion in the urine. Both hormones increase input of calcium and phosphorus from bone into the serum; both hormones also stimulate bone formation; vitamin D also increases absorption from the gut. Vitamin D decreases urinary excretion of both calcium and phosphorus, whereas PTH reduces calcium but increases phosphorus excretion. Calcitonin (CT) is a less critical hormone for calcium homeostasis, but in pharmacologic concentrations CT can reduce serum
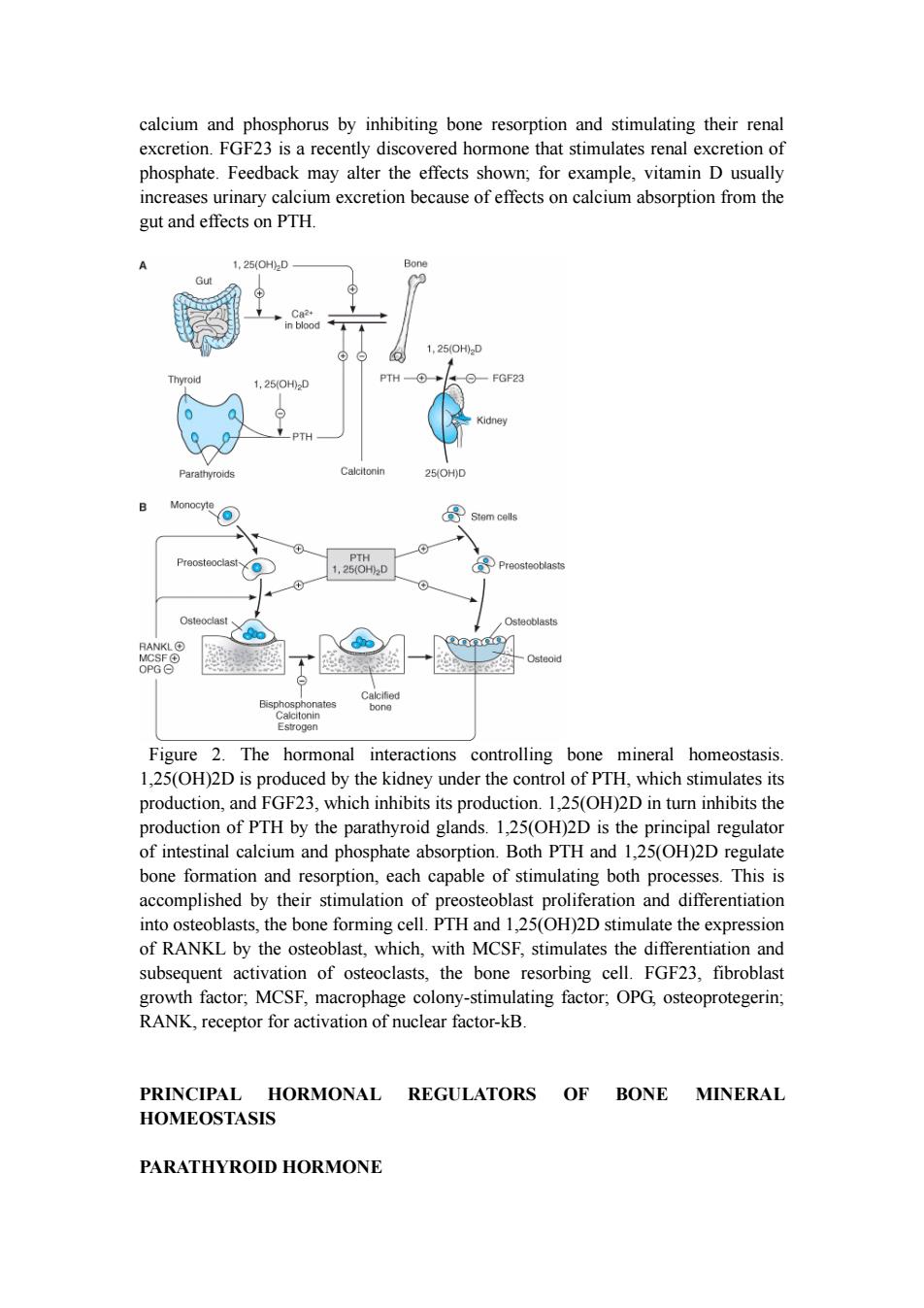
calcium and phosphorus by inhibiting bone resorption and stimulating their renal excretion.FGF23 is a recently discovered hormone that stimulates renal excretion of phosphate.Feedback may alter the effects shown;for example,vitamin D usually increases urinary calcium excretion because of effects on calcium absorption from the gut and effects on PTH. 1,25(OH2D Bon 1,25(0H0D Thy 1,25(0H02D PTH FGF23 Kidney PTH Parathyroids Calcitonin 25(OH)D Monocyte 导 Stem cells Preosteoclast PTH 1,25(0H02D Preosteoblasts Osteoclast Osteoblasts RANKLO Osteoid OPG⊙ Bisphosphonates Calcitonin Estrogen Figure 2.The hormonal interactions controlling bone mineral homeostasis. 1,25(OH)2D is produced by the kidney under the control of PTH,which stimulates its production,and FGF23,which inhibits its production.1,25(OH)2D in turn inhibits the production of PTH by the parathyroid glands.1,25(OH)2D is the principal regulator of intestinal calcium and phosphate absorption.Both PTH and 1,25(OH)2D regulate bone formation and resorption,each capable of stimulating both processes.This is accomplished by their stimulation of preosteoblast proliferation and differentiation into osteoblasts,the bone forming cell.PTH and 1,25(OH)2D stimulate the expression of RANKL by the osteoblast,which,with MCSF,stimulates the differentiation and subsequent activation of osteoclasts,the bone resorbing cell.FGF23,fibroblast growth factor;MCSF,macrophage colony-stimulating factor;OPG,osteoprotegerin; RANK,receptor for activation of nuclear factor-kB. PRINCIPAL HORMONAL REGULATORS OF BONE MINERAL HOMEOSTASIS PARATHYROID HORMONE
calcium and phosphorus by inhibiting bone resorption and stimulating their renal excretion. FGF23 is a recently discovered hormone that stimulates renal excretion of phosphate. Feedback may alter the effects shown; for example, vitamin D usually increases urinary calcium excretion because of effects on calcium absorption from the gut and effects on PTH. Figure 2. The hormonal interactions controlling bone mineral homeostasis. 1,25(OH)2D is produced by the kidney under the control of PTH, which stimulates its production, and FGF23, which inhibits its production. 1,25(OH)2D in turn inhibits the production of PTH by the parathyroid glands. 1,25(OH)2D is the principal regulator of intestinal calcium and phosphate absorption. Both PTH and 1,25(OH)2D regulate bone formation and resorption, each capable of stimulating both processes. This is accomplished by their stimulation of preosteoblast proliferation and differentiation into osteoblasts, the bone forming cell. PTH and 1,25(OH)2D stimulate the expression of RANKL by the osteoblast, which, with MCSF, stimulates the differentiation and subsequent activation of osteoclasts, the bone resorbing cell. FGF23, fibroblast growth factor; MCSF, macrophage colony-stimulating factor; OPG, osteoprotegerin; RANK, receptor for activation of nuclear factor-kB. PRINCIPAL HORMONAL REGULATORS OF BONE MINERAL HOMEOSTASIS PARATHYROID HORMONE
Parathyroid hormone(PTH)is a single-chain peptide hormone composed of 84 amino acids.It is produced in the parathyroid gland in a precursor form of 115 amino acids, the remaining 31 amino terminal amino acids being cleaved off before secretion. Within the gland is a calcium-sensitive protease capable of cleaving the intact hormone into fragments.Biologic activity resides in the amino terminal region such that synthetic 1-34 PTH is fully active.Loss of the first two amino terminal amino acids eliminates most biologic activity. The metabolic clearance of intact PTH is rapid,with a half-time of disappearance measured in minutes.Most of the clearance occurs in the liver and kidney.The biologically inactive carboxyl terminal fragments produced during metabolism of the intact hormone have a much lower clearance,especially in renal failure.This accounts in part for the very high PTH values often observed in the past in patients with renal failure when measured by radioimmunoassays directed against the carboxyl terminal region of the molecule.However,most PTH assays currently in use measure the intact hormone by a double antibody method,so that this circumstance is less frequently encountered in clinical practice.PTH regulates calcium and phosphate flux across cellular membranes in bone and kidney,resulting in increased serum calcium and decreased serum phosphate.In bone,PTH increases the activity and number of osteoclasts,the cells responsible for bone resorption.However,this stimulation of osteoclasts is not a direct effect.Rather,PTH acts on the osteoblast(the bone-forming cell)to induce a membrane-bound protein called RANK ligand(RANKL).This factor acts on osteoclasts and osteoclast precursors to increase both the numbers and the activity of osteoclasts.This action increases bone turnover or bone remodeling,a specific sequence of cellular events initiated by osteoclastic bone resorption and followed by osteoblastic bone formation.Although both bone resorption and bone formation are enhanced by PTH,the net effect of excess PTH is to increase bone resorption.PTH in low and intermittent doses increases bone formation without first stimulating bone resorption.This action appears to be indirect,involving other growth factors such as IGF-1.This has led to the recent approval of recombinant PTH 1-34 (teriparatide)for the treatment of osteoporosis.In the kidney,PTH increases the ability of the nephron to reabsorb calcium and magnesium but reduces its ability to reabsorb phosphate,amino acids,bicarbonate,sodium,chloride,and sulfate.Another important action of PTH on the kidney is its stimulation of 1,25-dihydroxyvitamin D (1,25[OH]2D)production. VITAMIN D Vitamin D is a secosteroid produced in the skin from 7-dehydrocholesterol under the influence of ultraviolet irradiation.Vitamin D is also found in certain foods and is used to supplement dairy products.Both the natural form(vitamin D3,cholecalciferol) and the plant-derived form(vitamin D2,ergocalciferol)are present in the diet.These forms differ in that ergocalciferol contains a double bond(C22-23)and an additional
Parathyroid hormone (PTH) is a single-chain peptide hormone composed of 84 amino acids. It is produced in the parathyroid gland in a precursor form of 115 amino acids, the remaining 31 amino terminal amino acids being cleaved off before secretion. Within the gland is a calcium-sensitive protease capable of cleaving the intact hormone into fragments. Biologic activity resides in the amino terminal region such that synthetic 1-34 PTH is fully active. Loss of the first two amino terminal amino acids eliminates most biologic activity. The metabolic clearance of intact PTH is rapid, with a half-time of disappearance measured in minutes. Most of the clearance occurs in the liver and kidney. The biologically inactive carboxyl terminal fragments produced during metabolism of the intact hormone have a much lower clearance, especially in renal failure. This accounts in part for the very high PTH values often observed in the past in patients with renal failure when measured by radioimmunoassays directed against the carboxyl terminal region of the molecule. However, most PTH assays currently in use measure the intact hormone by a double antibody method, so that this circumstance is less frequently encountered in clinical practice. PTH regulates calcium and phosphate flux across cellular membranes in bone and kidney, resulting in increased serum calcium and decreased serum phosphate. In bone, PTH increases the activity and number of osteoclasts, the cells responsible for bone resorption. However, this stimulation of osteoclasts is not a direct effect. Rather, PTH acts on the osteoblast (the bone-forming cell) to induce a membrane-bound protein called RANK ligand (RANKL). This factor acts on osteoclasts and osteoclast precursors to increase both the numbers and the activity of osteoclasts. This action increases bone turnover or bone remodeling, a specific sequence of cellular events initiated by osteoclastic bone resorption and followed by osteoblastic bone formation. Although both bone resorption and bone formation are enhanced by PTH, the net effect of excess PTH is to increase bone resorption. PTH in low and intermittent doses increases bone formation without first stimulating bone resorption. This action appears to be indirect, involving other growth factors such as IGF-1. This has led to the recent approval of recombinant PTH 1-34 (teriparatide) for the treatment of osteoporosis. In the kidney, PTH increases the ability of the nephron to reabsorb calcium and magnesium but reduces its ability to reabsorb phosphate, amino acids, bicarbonate, sodium, chloride, and sulfate. Another important action of PTH on the kidney is its stimulation of 1,25-dihydroxyvitamin D (1,25[OH]2D) production. VITAMIN D Vitamin D is a secosteroid produced in the skin from 7-dehydrocholesterol under the influence of ultraviolet irradiation. Vitamin D is also found in certain foods and is used to supplement dairy products. Both the natural form (vitamin D3, cholecalciferol) and the plant-derived form (vitamin D2, ergocalciferol) are present in the diet. These forms differ in that ergocalciferol contains a double bond (C22-23) and an additional
methyl group in the side chain(Figure 3).In humans,this difference apparently is of limited physiologic consequence (although ergocalciferol is less potent),and the following comments apply equally well to both forms of vitamin D. Vitamin D is a prohormone that serves as precursor to a number of biologically active metabolites (Figure 3).Vitamin D is first hydroxylated in the liver to form 25-hydroxyvitamin D(25[OH]D).This metabolite is further converted in the kidney to a number of other forms,the best-studied of which are 1,25-dihydroxyvitamin D (1,25[OH]2D)and 24,25-dihydroxyvitamin D (24,25[OH]2D).Of the natural metabolites,only vitamin D and 1,25(OH)2D (as calcitriol)are available for clinical use.Moreover,a number of analogs of 1,25(OH)2D are being synthesized to extend the usefulness of this metabolite to a variety of nonclassic conditions.Calcipotriene (calcipotriol),for example,is being used to treat psoriasis,a hyperproliferative skin disorder.Doxercalciferol and paricalcitol have recently been approved for the treatment of secondary hyperparathyroidism in patients with chronic kidney disease. Other analogs are being investigated for the treatment of various malignancies.The regulation of vitamin D metabolism is complex,involving calcium,phosphate,and a variety of hormones,the most important of which is PTH,which stimulates the production of 1,25(OH)2D by the kidney. Vitamin D and its metabolites circulate in plasma tightly bound to a carrier protein, the vitamin D-binding protein.This a-globulin binds 25(OH)D and 24,25(OH)2D with comparable high affinity and vitamin D and 1,25(OH)2D with lower affinity.In normal subjects,the terminal half-life of injected calcifediol is 23 days,whereas in anephric subjects it is 42 days.The half-life of 24,25(OH)2D is probably similar. Tracer studies with vitamin D have shown a rapid clearance from the blood.The liver appears to be the principal organ for clearance.Excess vitamin D is stored in adipose tissue.The metabolic clearance of calcitriol in humans indicates a rapid turnover,with a terminal half-life measured in hours.Several of the 1,25(OH)2D analogs are bound poorly by the vitamin D-binding protein.As a result,their clearance is very rapid, with a terminal half-life measured in minutes.Such analogs have little of the hypercalcemic,hypercalciuric effects of calcitriol,an important aspect of their use for the management of conditions such as psoriasis and hyperparathyroidism The mechanism of action of the vitamin D metabolites remains under active investigation.However,calcitriol is well established as the most potent agent with respect to stimulation of intestinal calcium and phosphate transport and bone resorption.Calcitriol appears to act on the intestine both by induction of new protein synthesis (eg,calcium-binding protein)and by modulation of calcium flux across the brush border and basolateral membranes by a means that does not require new protein synthesis.The molecular action of calcitriol on bone has received less attention. However,like PTH,calcitriol can induce RANK ligand in osteoblasts and proteins such as osteocalcin,which may regulate the mineralization process.The metabolites 25(OH)D and 24,25(OH)2D are far less potent stimulators of intestinal calcium and
methyl group in the side chain (Figure 3). In humans, this difference apparently is of limited physiologic consequence (although ergocalciferol is less potent), and the following comments apply equally well to both forms of vitamin D. Vitamin D is a prohormone that serves as precursor to a number of biologically active metabolites (Figure 3). Vitamin D is first hydroxylated in the liver to form 25-hydroxyvitamin D (25[OH]D). This metabolite is further converted in the kidney to a number of other forms, the best-studied of which are 1,25-dihydroxyvitamin D (1,25[OH]2D) and 24,25-dihydroxyvitamin D (24,25[OH]2D). Of the natural metabolites, only vitamin D and 1,25(OH)2D (as calcitriol) are available for clinical use. Moreover, a number of analogs of 1,25(OH)2D are being synthesized to extend the usefulness of this metabolite to a variety of nonclassic conditions. Calcipotriene (calcipotriol), for example, is being used to treat psoriasis, a hyperproliferative skin disorder. Doxercalciferol and paricalcitol have recently been approved for the treatment of secondary hyperparathyroidism in patients with chronic kidney disease. Other analogs are being investigated for the treatment of various malignancies. The regulation of vitamin D metabolism is complex, involving calcium, phosphate, and a variety of hormones, the most important of which is PTH, which stimulates the production of 1,25(OH)2D by the kidney. Vitamin D and its metabolites circulate in plasma tightly bound to a carrier protein, the vitamin D-binding protein. This a-globulin binds 25(OH)D and 24,25(OH)2D with comparable high affinity and vitamin D and 1,25(OH)2D with lower affinity. In normal subjects, the terminal half-life of injected calcifediol is 23 days, whereas in anephric subjects it is 42 days. The half-life of 24,25(OH)2D is probably similar. Tracer studies with vitamin D have shown a rapid clearance from the blood. The liver appears to be the principal organ for clearance. Excess vitamin D is stored in adipose tissue. The metabolic clearance of calcitriol in humans indicates a rapid turnover, with a terminal half-life measured in hours. Several of the 1,25(OH)2D analogs are bound poorly by the vitamin D-binding protein. As a result, their clearance is very rapid, with a terminal half-life measured in minutes. Such analogs have little of the hypercalcemic, hypercalciuric effects of calcitriol, an important aspect of their use for the management of conditions such as psoriasis and hyperparathyroidism. The mechanism of action of the vitamin D metabolites remains under active investigation. However, calcitriol is well established as the most potent agent with respect to stimulation of intestinal calcium and phosphate transport and bone resorption. Calcitriol appears to act on the intestine both by induction of new protein synthesis (eg, calcium-binding protein) and by modulation of calcium flux across the brush border and basolateral membranes by a means that does not require new protein synthesis. The molecular action of calcitriol on bone has received less attention. However, like PTH, calcitriol can induce RANK ligand in osteoblasts and proteins such as osteocalcin, which may regulate the mineralization process. The metabolites 25(OH)D and 24,25(OH)2D are far less potent stimulators of intestinal calcium and