Antipsychotic Agents Lithium William Z.Potter,MD,PhD,Leo E.Hollister,MD ANTIPSYCHOTIC AGENTS Introduction The terms antipsychotic and neuroleptic have been used interchangeably to denote a group of drugs that have been used mainly for treating schizophrenia but are also effective in some other psychoses and agitated states. History Antipsychotic drugs have been used in Western medicine for more than 50 years.Reserpine and chlorpromazine were the first drugs found to be useful in schizophrenia.Although chlorpromazine is still sometimes used for the treatment of psychoses,these forerunner drugs have been superseded by many newer agents.Their impact on psychiatry,however respecially on the treatment of schizophrenia has been enormous:The number of patients hospitalized in mental institutions has markedly decreased,and schizophrenia is now recognized as a biologic illness. Nature of Psychosis Schizophrenia The term "psychosis"denotes a variety of mental disorders.Schizophrenia is a particular kind of psychosis characterized mainly by a clear sensorium but a marked thinking disturbance. The pathogenesis of schizophrenia is unknown.Largely as a result of research stimulated by the discovery of antipsychotic drugs,a genetic predisposition has been proposed as a necessary but not always sufficient condition underlying psychotic disorder.This assumption has been supported by the observed familial incidence of schizophrenia.At least one gene that encoding neuregulin 1 is associated with schizophrenia in Icelandic and northern European populations.Additional genes associated with schizophrenia continue to be identified that may contribute to understanding the molecular basis for schizophrenia.Based on the efficacy of antipsychotic drugs,efforts continue to link the disorder with abnormalities of amine neurotransmitter function,especially that of dopamine (see Box:The Dopamine Hypothesis of Schizophrenia).The defects of this hypothesis are significant,and it is now appreciated that schizophrenia is far more complex than originally supposed
Antipsychotic Agents & Lithium William Z. Potter, MD, PhD, & Leo E. Hollister, MD I. ANTIPSYCHOTIC AGENTS Introduction The terms antipsychotic and neuroleptic have been used interchangeably to denote a group of drugs that have been used mainly for treating schizophrenia but are also effective in some other psychoses and agitated states. History Antipsychotic drugs have been used in Western medicine for more than 50 years. Reserpine and chlorpromazine were the first drugs found to be useful in schizophrenia. Although chlorpromazine is still sometimes used for the treatment of psychoses, these forerunner drugs have been superseded by many newer agents. Their impact on psychiatry, however respecially on the treatment of schizophrenia has been enormous: The number of patients hospitalized in mental institutions has markedly decreased, and schizophrenia is now recognized as a biologic illness. Nature of Psychosis & Schizophrenia The term "psychosis" denotes a variety of mental disorders. Schizophrenia is a particular kind of psychosis characterized mainly by a clear sensorium but a marked thinking disturbance. The pathogenesis of schizophrenia is unknown. Largely as a result of research stimulated by the discovery of antipsychotic drugs, a genetic predisposition has been proposed as a necessary but not always sufficient condition underlying psychotic disorder. This assumption has been supported by the observed familial incidence of schizophrenia. At least one gene that encoding neuregulin 1 is associated with schizophrenia in Icelandic and northern European populations. Additional genes associated with schizophrenia continue to be identified that may contribute to understanding the molecular basis for schizophrenia. Based on the efficacy of antipsychotic drugs, efforts continue to link the disorder with abnormalities of amine neurotransmitter function, especially that of dopamine (see Box: The Dopamine Hypothesis of Schizophrenia). The defects of this hypothesis are significant, and it is now appreciated that schizophrenia is far more complex than originally supposed

THE DOPAMINE HYPOTHESIS OF SCHIZOPHRENIA The dopamine hypothesis for schizophrenia is the most fully developed of several hypotheses and is the basis for much of the rationale for drug therapy. Several lines of circumstantial evidence suggest that excessive dopaminergic activity plays a role in the disorder:(1)many antipsychotic drugs strongly block postsynaptic D2 receptors in the central nervous system,especially in the mesolimbic-frontal system;(2)drugs that increase dopaminergic activity,such as levodopa (a precursor),amphetamines (releasers of dopamine),and apomorphine (a direct dopamine receptor agonist),either aggravate schizophrenia or produce psychosis de novo in some patients;(3)dopamine receptor density has been found postmortem to be increased in the brains of schizophrenics who have not been treated with antipsychotic drugs;(4) positron emission tomography(PET)has shown increased dopamine receptor density in both treated and untreated schizophrenics when compared with such scans of nonschizophrenic persons;and (5)successful treatment of schizophrenic patients has been reported to change the amount of homovanillic acid(HVA),a metabolite of dopamine,in the cerebrospinal fluid, plasma,and urine. The dopamine hypothesis is far from complete,however.If an abnormality of dopamine physiology were completely responsible for the pathogenesis of schizophrenia,antipsychotic drugs would do a much better job of treating patients%but they are only partially effective for most and ineffective for some patients.Moreover,it appears that antagonists of the NMDA receptor such as phencyclidine,when administered to nonpsychotic subjects,produce much more "schizophrenia-like"symptoms than do dopamine agonists.The cloning and characterization of multiple dopamine receptor types may permit more direct testing of the dopamine hypothesis if drugs can be developed that act more selectively on each receptor type.The traditional antipsychotics bind D2 50 times more avidly than Di or D3 receptors.Until recently,the main thrust in drug development was to find agents that were more potent and more selective in blocking D2 receptors.The fact that several of the atypical antipsychotic drugs have much less effect on D2 receptors and yet are effective in schizophrenia has redirected attention to the role of other dopamine receptors and to nondopamine receptors,especially serotonin receptor subtypes that may mediate synergistic effects or protect against the extrapyramidal consequences of D2 antagonism.As a result of these considerations,the direction of research has changed to a greater focus on compounds that may act on several transmitter-receptor systems.The great hope is to produce drugs with greater efficacy and fewer adverse effects,especially extrapyramidal toxicity
THE DOPAMINE HYPOTHESIS OF SCHIZOPHRENIA The dopamine hypothesis for schizophrenia is the most fully developed of several hypotheses and is the basis for much of the rationale for drug therapy. Several lines of circumstantial evidence suggest that excessive dopaminergic activity plays a role in the disorder: (1) many antipsychotic drugs strongly block postsynaptic D2 receptors in the central nervous system, especially in the mesolimbic-frontal system; (2) drugs that increase dopaminergic activity, such as levodopa (a precursor), amphetamines (releasers of dopamine), and apomorphine (a direct dopamine receptor agonist), either aggravate schizophrenia or produce psychosis de novo in some patients; (3) dopamine receptor density has been found postmortem to be increased in the brains of schizophrenics who have not been treated with antipsychotic drugs; (4) positron emission tomography (PET) has shown increased dopamine receptor density in both treated and untreated schizophrenics when compared with such scans of nonschizophrenic persons; and (5) successful treatment of schizophrenic patients has been reported to change the amount of homovanillic acid (HVA), a metabolite of dopamine, in the cerebrospinal fluid, plasma, and urine. The dopamine hypothesis is far from complete, however. If an abnormality of dopamine physiology were completely responsible for the pathogenesis of schizophrenia, antipsychotic drugs would do a much better job of treating patients¾but they are only partially effective for most and ineffective for some patients. Moreover, it appears that antagonists of the NMDA receptor such as phencyclidine, when administered to nonpsychotic subjects, produce much more "schizophrenia-like" symptoms than do dopamine agonists. The cloning and characterization of multiple dopamine receptor types may permit more direct testing of the dopamine hypothesis if drugs can be developed that act more selectively on each receptor type. The traditional antipsychotics bind D2 50 times more avidly than D1 or D3 receptors. Until recently, the main thrust in drug development was to find agents that were more potent and more selective in blocking D2 receptors. The fact that several of the atypical antipsychotic drugs have much less effect on D2 receptors and yet are effective in schizophrenia has redirected attention to the role of other dopamine receptors and to nondopamine receptors, especially serotonin receptor subtypes that may mediate synergistic effects or protect against the extrapyramidal consequences of D2 antagonism. As a result of these considerations, the direction of research has changed to a greater focus on compounds that may act on several transmitter-receptor systems. The great hope is to produce drugs with greater efficacy and fewer adverse effects, especially extrapyramidal toxicity

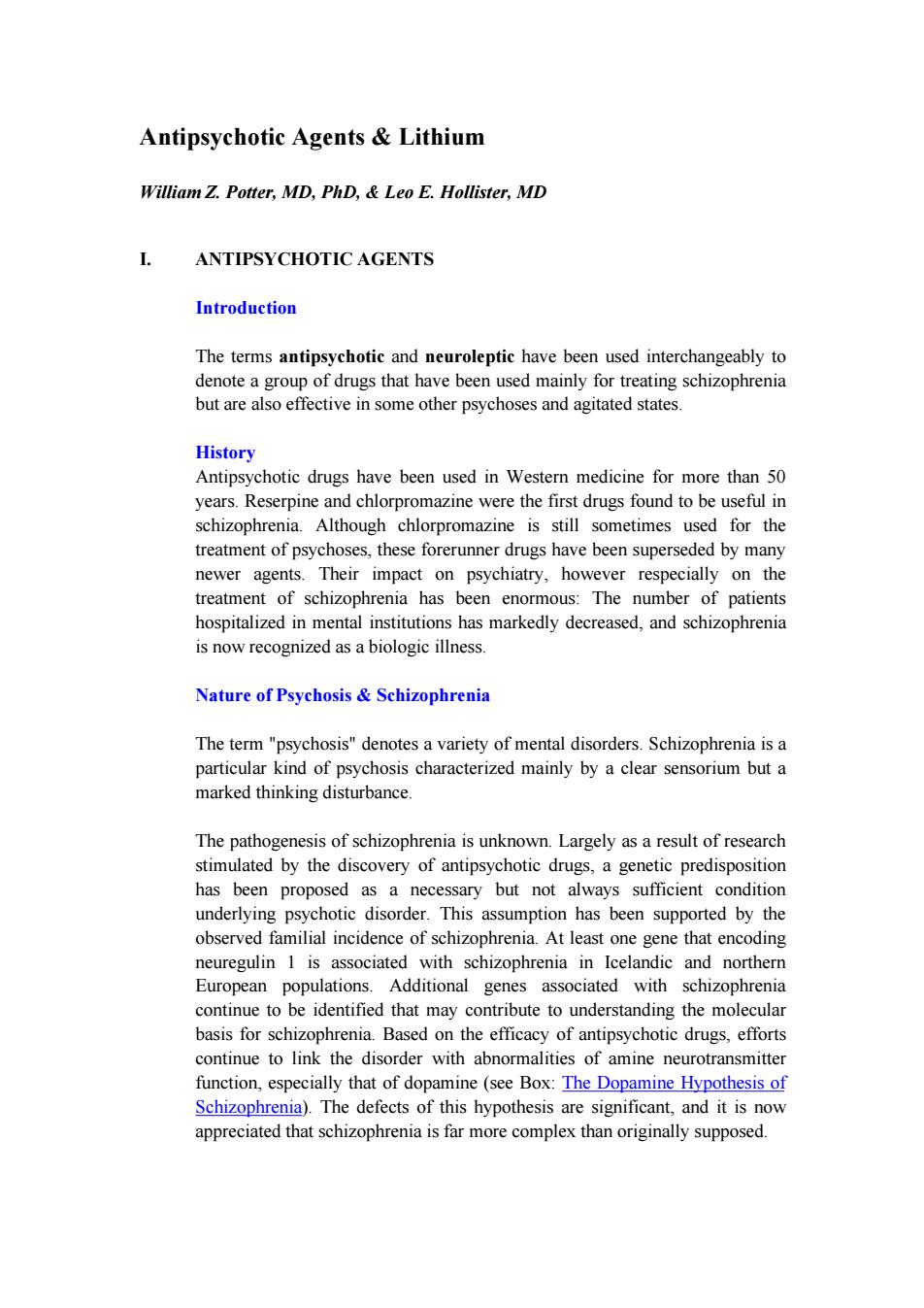
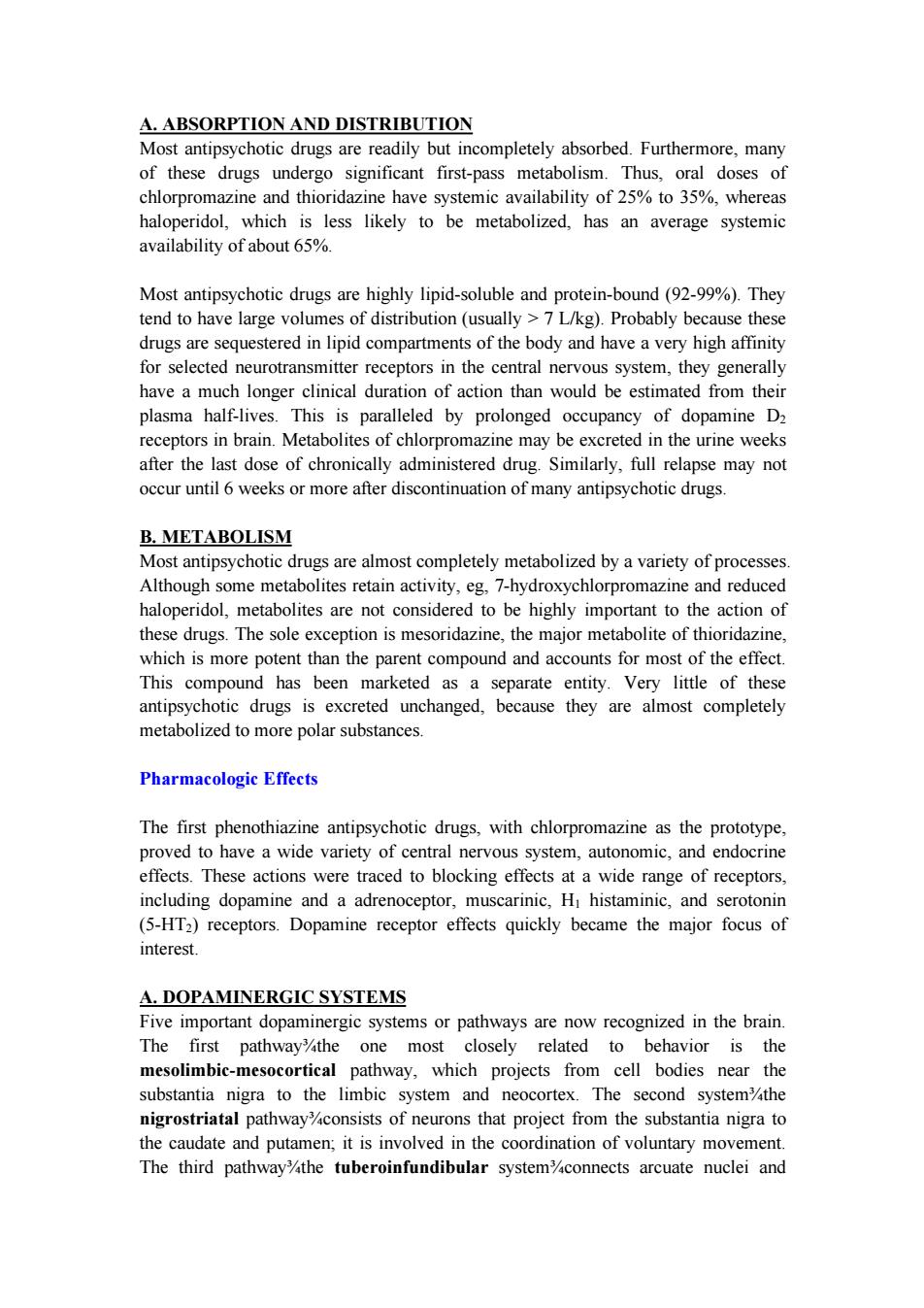
*Deceased BASIC PHARMACOLOGY OF ANTIPSYCHOTIC AGENTS Chemical Types A number of chemical structures have been associated with antipsychotic properties. The drugs can be classified into several groups as shown in Figures 29-1 and 29-2 A.PHENOTHIAZINE DERIVATIVES Three subfamilies of phenothiazines,based primarily on the side chain of the molecule,were once the most widely used of the antipsychotics.Aliphatic derivatives (eg,chlorpromazine)and piperidine derivatives (eg,thioridazine)are the least potent.Piperazine derivatives are more potent (effective in lower doses)but not necessarily more efficacious.The piperazine derivatives are also more selective in their pharmacologic effects. B.THIOXANTHENE DERIVATIVES This group of drugs is exemplified primarily by thiothixene.In general,these compounds are slightly less potent than their phenothiazine analogs. C.BUTYROPHENONE DERIVATIVES This group,of which haloperidol is the most widely used,has a very different structure from those of the two preceding groups.Diphenylbutylpiperidines are closely related compounds.The butyrophenones and congeners tend to be more potent and to have fewer autonomic effects but greater extrapyramidal effects. D.MISCELLANEOUS STRUCTURES The newer drugs,not all of which are available in the USA,have a variety of structures and include pimozide,molindone,loxapine,clozapine,olanzapine, quetiapine,risperidone,ziprasidone,and aripiprazole(Figure 29-2)
*Deceased BASIC PHARMACOLOGY OF ANTIPSYCHOTIC AGENTS Chemical Types A number of chemical structures have been associated with antipsychotic properties. The drugs can be classified into several groups as shown in Figures 29-1 and 29-2. A. PHENOTHIAZINE DERIVATIVES Three subfamilies of phenothiazines, based primarily on the side chain of the molecule, were once the most widely used of the antipsychotics. Aliphatic derivatives (eg, chlorpromazine) and piperidine derivatives (eg, thioridazine) are the least potent. Piperazine derivatives are more potent (effective in lower doses) but not necessarily more efficacious. The piperazine derivatives are also more selective in their pharmacologic effects. B. THIOXANTHENE DERIVATIVES This group of drugs is exemplified primarily by thiothixene. In general, these compounds are slightly less potent than their phenothiazine analogs. C. BUTYROPHENONE DERIVATIVES This group, of which haloperidol is the most widely used, has a very different structure from those of the two preceding groups. Diphenylbutylpiperidines are closely related compounds. The butyrophenones and congeners tend to be more potent and to have fewer autonomic effects but greater extrapyramidal effects. D. MISCELLANEOUS STRUCTURES The newer drugs, not all of which are available in the USA, have a variety of structures and include pimozide, molindone, loxapine, clozapine, olanzapine, quetiapine, risperidone, ziprasidone, and aripiprazole (Figure 29-2)

PHENOTHIAZINE DERIVATIVES THIOXANTHENE DERIVATIVE Phenothiazine 21 nucleus 12 10) Substituting C for N in the nucleus Aliphatic side chain Chlorpromazine (2)-CI 10-CH2-CHa-CH2-N-(CH) Thiothixene (2)-S02NCH,12 Thioridazine 2-SCH-C4一CH2 9=CH-CH一CH CH CH3 Piperazine side chain BUTYROPHENONE Trifluoperazine (2)-CF3 (10)-CH2-CH2-CH2 C-CH2-CH2-CH2- Perphenazine (2)-CI (10)-CH2-CHz-CH2 -CH2-CH2-OH Haloperidol Fluphenazine (2)-CF3 (10)-CH2-CH2-CH2- CH2-CH2-0H Figure 29-1.Structural formulas of some older antipsychotic drugs:phenothiazines, thioxanthenes,and butyrophenones.Only representative members of each type are shown. Ziprasidone Olanzapine Aripiprazole Figure 29-2.Structural formulas of some newer antipsychotic drugs. Pharmacokinetics
Figure 29-1. Structural formulas of some older antipsychotic drugs: phenothiazines, thioxanthenes, and butyrophenones. Only representative members of each type are shown. Figure 29-2. Structural formulas of some newer antipsychotic drugs. Pharmacokinetics
A.ABSORPTION AND DISTRIBUTION Most antipsychotic drugs are readily but incompletely absorbed.Furthermore,many of these drugs undergo significant first-pass metabolism.Thus,oral doses of chlorpromazine and thioridazine have systemic availability of 25%to 35%,whereas haloperidol,which is less likely to be metabolized,has an average systemic availability of about 65%. Most antipsychotic drugs are highly lipid-soluble and protein-bound(92-99%).They tend to have large volumes of distribution(usually >7 L/kg).Probably because these drugs are sequestered in lipid compartments of the body and have a very high affinity for selected neurotransmitter receptors in the central nervous system,they generally have a much longer clinical duration of action than would be estimated from their plasma half-lives.This is paralleled by prolonged occupancy of dopamine D2 receptors in brain.Metabolites of chlorpromazine may be excreted in the urine weeks after the last dose of chronically administered drug.Similarly,full relapse may not occur until 6 weeks or more after discontinuation of many antipsychotic drugs. B.METABOLISM Most antipsychotic drugs are almost completely metabolized by a variety of processes. Although some metabolites retain activity,eg,7-hydroxychlorpromazine and reduced haloperidol,metabolites are not considered to be highly important to the action of these drugs.The sole exception is mesoridazine,the major metabolite of thioridazine, which is more potent than the parent compound and accounts for most of the effect. This compound has been marketed as a separate entity.Very little of these antipsychotic drugs is excreted unchanged,because they are almost completely metabolized to more polar substances. Pharmacologic Effects The first phenothiazine antipsychotic drugs,with chlorpromazine as the prototype, proved to have a wide variety of central nervous system,autonomic,and endocrine effects.These actions were traced to blocking effects at a wide range of receptors, including dopamine and a adrenoceptor,muscarinic,Hi histaminic,and serotonin (5-HT2)receptors.Dopamine receptor effects quickly became the major focus of interest. A.DOPAMINERGIC SYSTEMS Five important dopaminergic systems or pathways are now recognized in the brain. The first pathway%the one most closely related to behavior is the mesolimbic-mesocortical pathway,which projects from cell bodies near the substantia nigra to the limbic system and neocortex.The second system%the nigrostriatal pathwayconsists of neurons that project from the substantia nigra to the caudate and putamen;it is involved in the coordination of voluntary movement. The third pathwaythe tuberoinfundibular system'connects arcuate nuclei and
A. ABSORPTION AND DISTRIBUTION Most antipsychotic drugs are readily but incompletely absorbed. Furthermore, many of these drugs undergo significant first-pass metabolism. Thus, oral doses of chlorpromazine and thioridazine have systemic availability of 25% to 35%, whereas haloperidol, which is less likely to be metabolized, has an average systemic availability of about 65%. Most antipsychotic drugs are highly lipid-soluble and protein-bound (92-99%). They tend to have large volumes of distribution (usually > 7 L/kg). Probably because these drugs are sequestered in lipid compartments of the body and have a very high affinity for selected neurotransmitter receptors in the central nervous system, they generally have a much longer clinical duration of action than would be estimated from their plasma half-lives. This is paralleled by prolonged occupancy of dopamine D2 receptors in brain. Metabolites of chlorpromazine may be excreted in the urine weeks after the last dose of chronically administered drug. Similarly, full relapse may not occur until 6 weeks or more after discontinuation of many antipsychotic drugs. B. METABOLISM Most antipsychotic drugs are almost completely metabolized by a variety of processes. Although some metabolites retain activity, eg, 7-hydroxychlorpromazine and reduced haloperidol, metabolites are not considered to be highly important to the action of these drugs. The sole exception is mesoridazine, the major metabolite of thioridazine, which is more potent than the parent compound and accounts for most of the effect. This compound has been marketed as a separate entity. Very little of these antipsychotic drugs is excreted unchanged, because they are almost completely metabolized to more polar substances. Pharmacologic Effects The first phenothiazine antipsychotic drugs, with chlorpromazine as the prototype, proved to have a wide variety of central nervous system, autonomic, and endocrine effects. These actions were traced to blocking effects at a wide range of receptors, including dopamine and a adrenoceptor, muscarinic, H1 histaminic, and serotonin (5-HT2) receptors. Dopamine receptor effects quickly became the major focus of interest. A. DOPAMINERGIC SYSTEMS Five important dopaminergic systems or pathways are now recognized in the brain. The first pathway¾the one most closely related to behavior is the mesolimbic-mesocortical pathway, which projects from cell bodies near the substantia nigra to the limbic system and neocortex. The second system¾the nigrostriatal pathway¾consists of neurons that project from the substantia nigra to the caudate and putamen; it is involved in the coordination of voluntary movement. The third pathway¾the tuberoinfundibular system¾connects arcuate nuclei and