English Reading Materials Chapter 27:Histamine INTRODUCTION Histamine and serotonin(5-hydroxytryptamine)are biologically active amines that function as neurotransmitters and are found in non-neural tissues,have complex physiologic and pathologic effects through multiple receptor subtypes,and are often released locally.Together with endogenous peptides,prostaglandins and leukotrienes, and cytokines,they are sometimes called autacoids (Greek,"self-remedy")or local hormones in recognition of these properties. Because of their broad and largely undesirable effects,neither histamine nor serotonin has any clinical application in the treatment of disease.However,compounds that selectively activate certain receptor subtypes or selectively antagonize the actions of these amines are of considerable clinical usefulness.This chapter therefore emphasizes the basic pharmacology of the agonist amines and the clinical pharmacology of the more selective agonist and antagonist drugs.The ergot alkaloids, compounds with partial agonist activity at serotonin and several other receptors,are discussed at the end of the chapter. I.HISTAMINE INTRODUCTION Histamine was synthesized in 1907 and later isolated from mammalian tissues.Early hypotheses concerning the possible physiologic roles of tissue histamine were based on similarities between the effects of intravenously administered histamine and the symptoms of anaphylactic shock and tissue injury.Marked species variation is observed,but in humans histamine is an important mediator of immediate allergic and inflammatory reactions,although it plays only a modest role in anaphylaxis. Histamine plays an important role in gastric acid secretion and functions as a neurotransmitter and neuromodulator.Newer evidence indicates that histamine also plays a role in chemotaxis of white blood cells. BASIC PHARMACOLOGY OF HISTAMINE Chemistry Pharmacokinetics Histamine occurs in plants as well as in animal tissues and is a component of some venoms and stinging secretions
English Reading Materials Chapter 27: Histamine INTRODUCTION Histamine and serotonin (5-hydroxytryptamine) are biologically active amines that function as neurotransmitters and are found in non-neural tissues, have complex physiologic and pathologic effects through multiple receptor subtypes, and are often released locally. Together with endogenous peptides, prostaglandins and leukotrienes, and cytokines, they are sometimes called autacoids (Greek, "self-remedy") or local hormones in recognition of these properties. Because of their broad and largely undesirable effects, neither histamine nor serotonin has any clinical application in the treatment of disease. However, compounds that selectively activate certain receptor subtypes or selectively antagonize the actions of these amines are of considerable clinical usefulness. This chapter therefore emphasizes the basic pharmacology of the agonist amines and the clinical pharmacology of the more selective agonist and antagonist drugs. The ergot alkaloids, compounds with partial agonist activity at serotonin and several other receptors, are discussed at the end of the chapter. I. HISTAMINE INTRODUCTION Histamine was synthesized in 1907 and later isolated from mammalian tissues. Early hypotheses concerning the possible physiologic roles of tissue histamine were based on similarities between the effects of intravenously administered histamine and the symptoms of anaphylactic shock and tissue injury. Marked species variation is observed, but in humans histamine is an important mediator of immediate allergic and inflammatory reactions, although it plays only a modest role in anaphylaxis. Histamine plays an important role in gastric acid secretion and functions as a neurotransmitter and neuromodulator. Newer evidence indicates that histamine also plays a role in chemotaxis of white blood cells. BASIC PHARMACOLOGY OF HISTAMINE Chemistry Pharmacokinetics Histamine occurs in plants as well as in animal tissues and is a component of some venoms and stinging secretions
Histamine is formed by decarboxylation of the amino acid /-histidine,a reaction catalyzed in mammalian tissues by the enzyme histidine decarboxylase.Once formed, histamine is either stored or rapidly inactivated.Very little histamine is excreted unchanged.The major metabolic pathways involve conversion to N-methylhistamine, methylimidazoleacetic acid,and imidazoleacetic acid (IAA).Certain neoplasms (systemic mastocytosis,urticaria pigmentosa,gastric carcinoid,and occasionally myelogenous leukemia)are associated with increased numbers of mast cells or basophils and with increased excretion of histamine and its metabolites. Most tissue histamine is sequestered and bound in granules(vesicles)in mast cells or basophils;the histamine content of many tissues is directly related to their mast cell content.The bound form of histamine is biologically inactive,but many stimuli,as noted below,can trigger the release of mast cell histamine,allowing the free amine to exert its actions on surrounding tissues.Mast cells are especially rich at sites of potential tissue injury nose,mouth,and feet;internal body surfaces;and blood vessels,particularly at pressure points and bifurcations. Non-mast cell histamine is found in several tissues,including the brain,where it functions as a neurotransmitter.Endogenous neurotransmitter histamine may play a role in many brain functions such as neuroendocrine control,cardiovascular regulation,thermal and body weight regulation,and arousal. A second important nonneuronal site of histamine storage and release is the enterochromaffin-like (ECL)cells of the fundus of the stomach.ECL cells release histamine,one of the primary gastric acid secretagogues,to activate the acid-producing parietal cells of the mucosa. Storage Release of Histamine The stores of histamine in mast cells can be released through several mechanisms A.IMMUNOLOGIC RELEASE Immunologic processes account for the most important pathophysiologic mechanism of mast cell and basophil histamine release.These cells,if sensitized by IgE antibodies attached to their surface membranes,degranulate "explosively"when exposed to the appropriate antigen(see Figure 1,effector phase).This type of release also requires energy and calcium.Degranulation leads to the simultaneous release of histamine,adenosine triphosphate (ATP),and other mediators that are stored together in the granules.Histamine released by this mechanism is a mediator in immediate (type I)allergic reactions.Substances released during IgG-or IgM-mediated immune
Histamine is formed by decarboxylation of the amino acid l-histidine, a reaction catalyzed in mammalian tissues by the enzyme histidine decarboxylase. Once formed, histamine is either stored or rapidly inactivated. Very little histamine is excreted unchanged. The major metabolic pathways involve conversion to N-methylhistamine, methylimidazoleacetic acid, and imidazoleacetic acid (IAA). Certain neoplasms (systemic mastocytosis, urticaria pigmentosa, gastric carcinoid, and occasionally myelogenous leukemia) are associated with increased numbers of mast cells or basophils and with increased excretion of histamine and its metabolites. Most tissue histamine is sequestered and bound in granules (vesicles) in mast cells or basophils; the histamine content of many tissues is directly related to their mast cell content. The bound form of histamine is biologically inactive, but many stimuli, as noted below, can trigger the release of mast cell histamine, allowing the free amine to exert its actions on surrounding tissues. Mast cells are especially rich at sites of potential tissue injury nose, mouth, and feet; internal body surfaces; and blood vessels, particularly at pressure points and bifurcations. Non-mast cell histamine is found in several tissues, including the brain, where it functions as a neurotransmitter. Endogenous neurotransmitter histamine may play a role in many brain functions such as neuroendocrine control, cardiovascular regulation, thermal and body weight regulation, and arousal. A second important nonneuronal site of histamine storage and release is the enterochromaffin-like (ECL) cells of the fundus of the stomach. ECL cells release histamine, one of the primary gastric acid secretagogues, to activate the acid-producing parietal cells of the mucosa. Storage Release of Histamine The stores of histamine in mast cells can be released through several mechanisms. A. IMMUNOLOGIC RELEASE Immunologic processes account for the most important pathophysiologic mechanism of mast cell and basophil histamine release. These cells, if sensitized by IgE antibodies attached to their surface membranes, degranulate "explosively" when exposed to the appropriate antigen (see Figure 1, effector phase). This type of release also requires energy and calcium. Degranulation leads to the simultaneous release of histamine, adenosine triphosphate (ATP), and other mediators that are stored together in the granules. Histamine released by this mechanism is a mediator in immediate (type I) allergic reactions. Substances released during IgG- or IgM-mediated immune
reactions that activate the complement cascade also release histamine from mast cells and basophils. By a negative feedback control mechanism mediated by H2 receptors,histamine appears to modulate its own release and that of other mediators from sensitized mast cells in some tissues.In humans,mast cells in skin and basophils show this negative feedback mechanism;lung mast cells do not.Thus,histamine may act to limit the intensity of the allergic reaction in the skin and blood. Endogenous histamine has a modulating role in a variety of inflammatory and immune responses.Upon injury to a tissue,released histamine causes local vasodilation and leakage of plasma containing mediators of acute inflammation (complement,C-reactive protein),and antibodies.Histamine has an active chemotactic attraction for inflammatory cells (neutrophils,eosinophils,basophils, monocytes,and lymphocytes).Histamine inhibits the release of lysosome contents and several T-and B-lymphocyte functions.Most of these actions are mediated by H2 or H4 receptors.Release of peptides from nerves in response to inflammation is also probably modulated by histamine,in this case acting through presynaptic H3 receptors. B.CHEMICAL AND MECHANICAL RELEASE Certain amines,including drugs such as morphine and tubocurarine,can displace histamine from the heparin-protein complex within cells.This type of release does not require energy and is not associated with mast cell injury or degranulation.Loss of granules from the mast cell also releases histamine,since sodium ions in the extracellular fluid rapidly displace the amine from the complex.Chemical and mechanical mast cell injury causes degranulation and histamine release.Compound 48/80,an experimental drug,selectively releases histamine from tissue mast cells by an exocytotic degranulation process requiring energy and calcium
reactions that activate the complement cascade also release histamine from mast cells and basophils. By a negative feedback control mechanism mediated by H2 receptors, histamine appears to modulate its own release and that of other mediators from sensitized mast cells in some tissues. In humans, mast cells in skin and basophils show this negative feedback mechanism; lung mast cells do not. Thus, histamine may act to limit the intensity of the allergic reaction in the skin and blood. Endogenous histamine has a modulating role in a variety of inflammatory and immune responses. Upon injury to a tissue, released histamine causes local vasodilation and leakage of plasma containing mediators of acute inflammation (complement, C-reactive protein), and antibodies. Histamine has an active chemotactic attraction for inflammatory cells (neutrophils, eosinophils, basophils, monocytes, and lymphocytes). Histamine inhibits the release of lysosome contents and several T- and B-lymphocyte functions. Most of these actions are mediated by H2 or H4 receptors. Release of peptides from nerves in response to inflammation is also probably modulated by histamine, in this case acting through presynaptic H3 receptors. B. CHEMICAL AND MECHANICAL RELEASE Certain amines, including drugs such as morphine and tubocurarine, can displace histamine from the heparin-protein complex within cells. This type of release does not require energy and is not associated with mast cell injury or degranulation. Loss of granules from the mast cell also releases histamine, since sodium ions in the extracellular fluid rapidly displace the amine from the complex. Chemical and mechanical mast cell injury causes degranulation and histamine release. Compound 48/80, an experimental drug, selectively releases histamine from tissue mast cells by an exocytotic degranulation process requiring energy and calcium
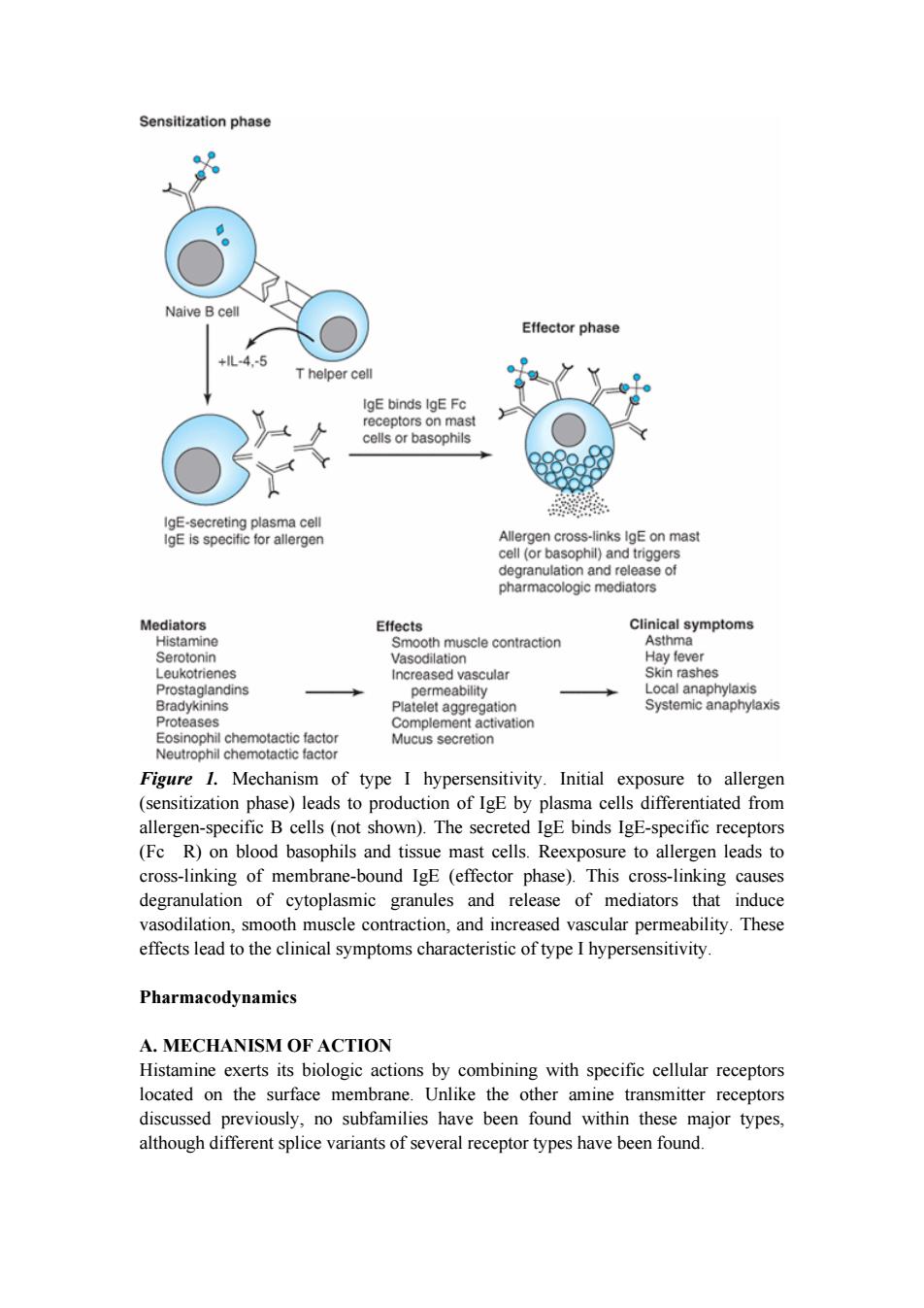
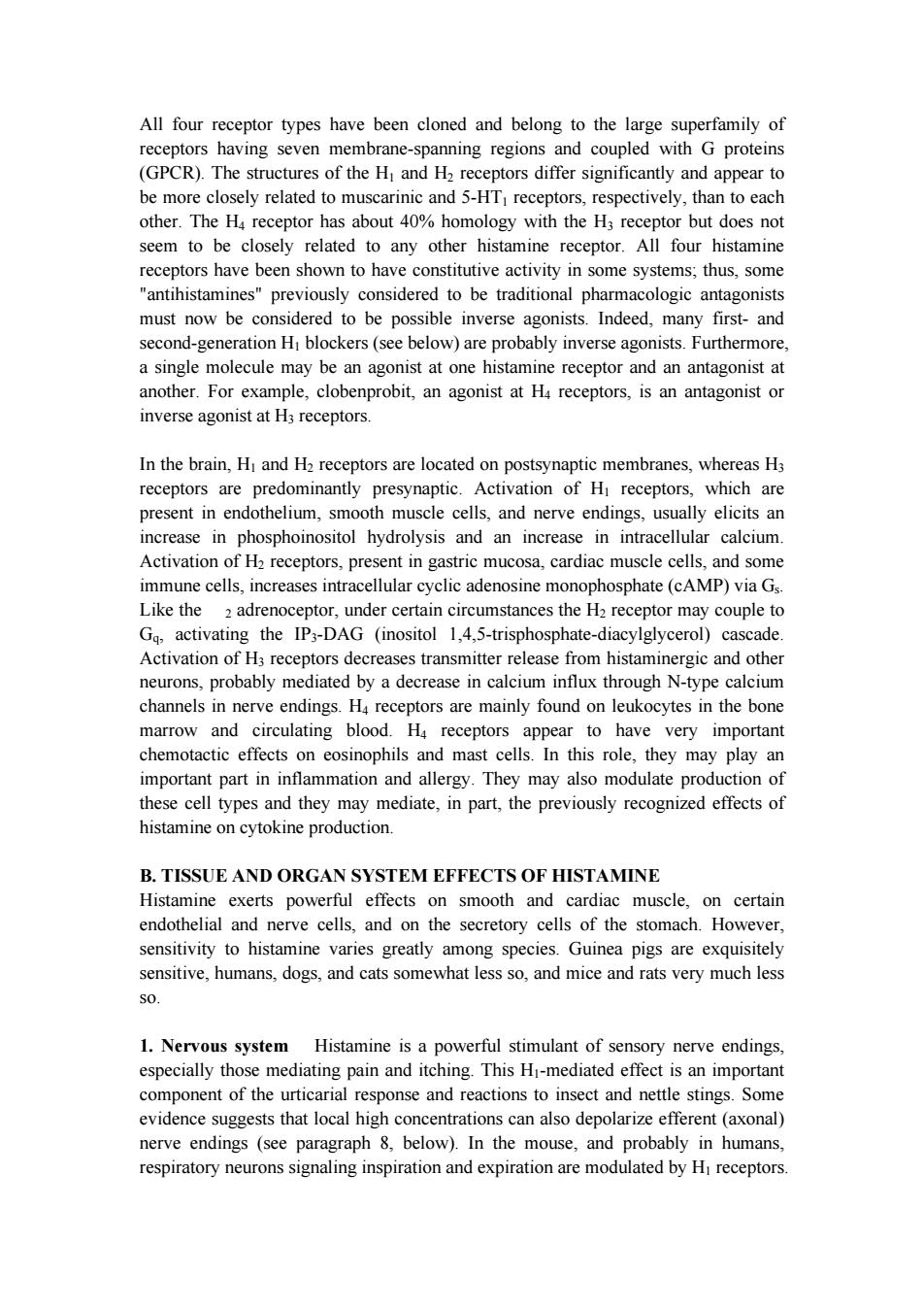
Sensitization phase Naive Bcell Effector phase +lL-4-5 T helper cell IgE binds IgE Fc receptors on mast cells or basophils IgE-secreting plasma cell IgE is specific for allergen Allergen cross-links IgE on mast cell (or basophil)and triggers degranulation and release of pharmacologic mediators Mediators Effects Clinical symptoms Histamine Smooth muscle contraction Asthma Serotonin Vasodilation Hay fever Leukotrienes Increased vascular Skin rashes Prostaglandins permeability Local anaphylaxis Bradykinins Platelet aggregation Systemic anaphylaxis Proteases Complement activation Eosinophil chemotactic factor Mucus secretion Neutrophil chemotactic factor Figure 1.Mechanism of type I hypersensitivity.Initial exposure to allergen (sensitization phase)leads to production of IgE by plasma cells differentiated from allergen-specific B cells(not shown).The secreted IgE binds IgE-specific receptors (Fc R)on blood basophils and tissue mast cells.Reexposure to allergen leads to cross-linking of membrane-bound IgE (effector phase).This cross-linking causes degranulation of cytoplasmic granules and release of mediators that induce vasodilation,smooth muscle contraction,and increased vascular permeability.These effects lead to the clinical symptoms characteristic of type I hypersensitivity Pharmacodynamics A.MECHANISM OF ACTION Histamine exerts its biologic actions by combining with specific cellular receptors located on the surface membrane.Unlike the other amine transmitter receptors discussed previously,no subfamilies have been found within these major types, although different splice variants of several receptor types have been found
Figure 1. Mechanism of type I hypersensitivity. Initial exposure to allergen (sensitization phase) leads to production of IgE by plasma cells differentiated from allergen-specific B cells (not shown). The secreted IgE binds IgE-specific receptors (Fc R) on blood basophils and tissue mast cells. Reexposure to allergen leads to cross-linking of membrane-bound IgE (effector phase). This cross-linking causes degranulation of cytoplasmic granules and release of mediators that induce vasodilation, smooth muscle contraction, and increased vascular permeability. These effects lead to the clinical symptoms characteristic of type I hypersensitivity. Pharmacodynamics A. MECHANISM OF ACTION Histamine exerts its biologic actions by combining with specific cellular receptors located on the surface membrane. Unlike the other amine transmitter receptors discussed previously, no subfamilies have been found within these major types, although different splice variants of several receptor types have been found
All four receptor types have been cloned and belong to the large superfamily of receptors having seven membrane-spanning regions and coupled with G proteins (GPCR).The structures of the H and H2 receptors differ significantly and appear to be more closely related to muscarinic and 5-HTI receptors,respectively,than to each other.The H4 receptor has about 40%homology with the H3 receptor but does not seem to be closely related to any other histamine receptor.All four histamine receptors have been shown to have constitutive activity in some systems;thus,some "antihistamines"previously considered to be traditional pharmacologic antagonists must now be considered to be possible inverse agonists.Indeed,many first-and second-generation HI blockers(see below)are probably inverse agonists.Furthermore, a single molecule may be an agonist at one histamine receptor and an antagonist at another.For example,clobenprobit,an agonist at H4 receptors,is an antagonist or inverse agonist at H3 receptors. In the brain,Hi and H2 receptors are located on postsynaptic membranes,whereas H3 receptors are predominantly presynaptic.Activation of Hi receptors,which are present in endothelium,smooth muscle cells,and nerve endings,usually elicits an increase in phosphoinositol hydrolysis and an increase in intracellular calcium. Activation of H2 receptors,present in gastric mucosa,cardiac muscle cells,and some immune cells,increases intracellular cyclic adenosine monophosphate(cAMP)via Gs. Like the 2 adrenoceptor,under certain circumstances the H2 receptor may couple to Gq,activating the IP3-DAG (inositol 1,4,5-trisphosphate-diacylglycerol)cascade. Activation of H3 receptors decreases transmitter release from histaminergic and other neurons,probably mediated by a decrease in calcium influx through N-type calcium channels in nerve endings.H4 receptors are mainly found on leukocytes in the bone marrow and circulating blood.H4 receptors appear to have very important chemotactic effects on eosinophils and mast cells.In this role,they may play an important part in inflammation and allergy.They may also modulate production of these cell types and they may mediate,in part,the previously recognized effects of histamine on cytokine production. B.TISSUE AND ORGAN SYSTEM EFFECTS OF HISTAMINE Histamine exerts powerful effects on smooth and cardiac muscle,on certain endothelial and nerve cells,and on the secretory cells of the stomach.However, sensitivity to histamine varies greatly among species.Guinea pigs are exquisitely sensitive,humans,dogs,and cats somewhat less so,and mice and rats very much less SO 1.Nervous system Histamine is a powerful stimulant of sensory nerve endings, especially those mediating pain and itching.This Hi-mediated effect is an important component of the urticarial response and reactions to insect and nettle stings.Some evidence suggests that local high concentrations can also depolarize efferent(axonal) nerve endings (see paragraph 8,below).In the mouse,and probably in humans, respiratory neurons signaling inspiration and expiration are modulated by Hi receptors
All four receptor types have been cloned and belong to the large superfamily of receptors having seven membrane-spanning regions and coupled with G proteins (GPCR). The structures of the H1 and H2 receptors differ significantly and appear to be more closely related to muscarinic and 5-HT1 receptors, respectively, than to each other. The H4 receptor has about 40% homology with the H3 receptor but does not seem to be closely related to any other histamine receptor. All four histamine receptors have been shown to have constitutive activity in some systems; thus, some "antihistamines" previously considered to be traditional pharmacologic antagonists must now be considered to be possible inverse agonists. Indeed, many first- and second-generation H1 blockers (see below) are probably inverse agonists. Furthermore, a single molecule may be an agonist at one histamine receptor and an antagonist at another. For example, clobenprobit, an agonist at H4 receptors, is an antagonist or inverse agonist at H3 receptors. In the brain, H1 and H2 receptors are located on postsynaptic membranes, whereas H3 receptors are predominantly presynaptic. Activation of H1 receptors, which are present in endothelium, smooth muscle cells, and nerve endings, usually elicits an increase in phosphoinositol hydrolysis and an increase in intracellular calcium. Activation of H2 receptors, present in gastric mucosa, cardiac muscle cells, and some immune cells, increases intracellular cyclic adenosine monophosphate (cAMP) via Gs. Like the 2 adrenoceptor, under certain circumstances the H2 receptor may couple to Gq, activating the IP3-DAG (inositol 1,4,5-trisphosphate-diacylglycerol) cascade. Activation of H3 receptors decreases transmitter release from histaminergic and other neurons, probably mediated by a decrease in calcium influx through N-type calcium channels in nerve endings. H4 receptors are mainly found on leukocytes in the bone marrow and circulating blood. H4 receptors appear to have very important chemotactic effects on eosinophils and mast cells. In this role, they may play an important part in inflammation and allergy. They may also modulate production of these cell types and they may mediate, in part, the previously recognized effects of histamine on cytokine production. B. TISSUE AND ORGAN SYSTEM EFFECTS OF HISTAMINE Histamine exerts powerful effects on smooth and cardiac muscle, on certain endothelial and nerve cells, and on the secretory cells of the stomach. However, sensitivity to histamine varies greatly among species. Guinea pigs are exquisitely sensitive, humans, dogs, and cats somewhat less so, and mice and rats very much less so. 1. Nervous system Histamine is a powerful stimulant of sensory nerve endings, especially those mediating pain and itching. This H1-mediated effect is an important component of the urticarial response and reactions to insect and nettle stings. Some evidence suggests that local high concentrations can also depolarize efferent (axonal) nerve endings (see paragraph 8, below). In the mouse, and probably in humans, respiratory neurons signaling inspiration and expiration are modulated by H1 receptors