
English Reading Materials Chapter 21:Vasodilators the Treatment of Angina Pectoris INTRODUCTION Angina pectoris is the most common condition involving tissue ischemia in which vasodilator drugs are used.The name denotes chest pain caused by accumulation of metabolites resulting from myocardial ischemia.The organic nitrates,eg, nitroglycerin,are the mainstay of therapy for the immediate relief of angina.Another group of vasodilators,the calcium channel blockers,is also important,especially for prophylaxis,and the blockers,which are not vasodilators,are also useful in prophylaxis.New groups of drugs under investigation include fatty acid oxidation inhibitors and selective cardiac rate inhibitors. Ischemic heart disease is the most common serious health problem in many Western societies.By far the most frequent cause of angina is atheromatous obstruction of the large coronary vessels (atherosclerotic angina,classic angina).However,transient spasm of localized portions of these vessels,which is usually associated with underlying atheromas,can also cause significant myocardial ischemia and pain (vasospastic or variant angina). The primary cause of angina pectoris is an imbalance between the oxygen requirement of the heart and the oxygen supplied to it via the coronary vessels.In classic angina,the imbalance occurs when the myocardial oxygen requirement increases,as during exercise,and coronary blood flow does not increase proportionately.The resulting ischemia usually leads to pain.Classic angina is therefore "angina of effort."(In some individuals,the ischemia is not always accompanied by pain,resulting in "silent"or "ambulatory"ischemia.)In variant angina,oxygen delivery decreases as a result of reversible coronary vasospasm. Variant angina is also called Prinzmetal's angina. In theory,the imbalance between oxygen delivery and myocardial oxygen demand can be corrected by decreasing oxygen demand or by increasing delivery (by increasing coronary flow).In effort angina,oxygen demand can be reduced by decreasing cardiac work or,according to recent studies,by shifting myocardial metabolism to substrates that require less oxygen per unit of ATP produced.In variant angina,on the other hand,spasm of coronary vessels can be reversed by nitrates or calcium channel blockers.Lipid-lowering drugs,especially the "statins,"have become extremely important in the long-term treatment of atherosclerotic disease. 1
1 English Reading Materials Chapter 21: Vasodilators the Treatment of Angina Pectoris INTRODUCTION Angina pectoris is the most common condition involving tissue ischemia in which vasodilator drugs are used. The name denotes chest pain caused by accumulation of metabolites resulting from myocardial ischemia. The organic nitrates, eg, nitroglycerin, are the mainstay of therapy for the immediate relief of angina. Another group of vasodilators, the calcium channel blockers, is also important, especially for prophylaxis, and the blockers, which are not vasodilators, are also useful in prophylaxis. New groups of drugs under investigation include fatty acid oxidation inhibitors and selective cardiac rate inhibitors. Ischemic heart disease is the most common serious health problem in many Western societies. By far the most frequent cause of angina is atheromatous obstruction of the large coronary vessels (atherosclerotic angina, classic angina). However, transient spasm of localized portions of these vessels, which is usually associated with underlying atheromas, can also cause significant myocardial ischemia and pain (vasospastic or variant angina). The primary cause of angina pectoris is an imbalance between the oxygen requirement of the heart and the oxygen supplied to it via the coronary vessels. In classic angina, the imbalance occurs when the myocardial oxygen requirement increases, as during exercise, and coronary blood flow does not increase proportionately. The resulting ischemia usually leads to pain. Classic angina is therefore "angina of effort." (In some individuals, the ischemia is not always accompanied by pain, resulting in "silent" or "ambulatory" ischemia.) In variant angina, oxygen delivery decreases as a result of reversible coronary vasospasm. Variant angina is also called Prinzmetal's angina. In theory, the imbalance between oxygen delivery and myocardial oxygen demand can be corrected by decreasing oxygen demand or by increasing delivery (by increasing coronary flow). In effort angina, oxygen demand can be reduced by decreasing cardiac work or, according to recent studies, by shifting myocardial metabolism to substrates that require less oxygen per unit of ATP produced. In variant angina, on the other hand, spasm of coronary vessels can be reversed by nitrates or calcium channel blockers. Lipid-lowering drugs, especially the "statins," have become extremely important in the long-term treatment of atherosclerotic disease

Unstable angina,an acute coronary syndrome,is said to be present when there are episodes of angina at rest and when there is a change in the character,frequency,and duration of chest pain as well as precipitating factors in patients with previously stable angina.Unstable angina is caused by episodes of increased epicardial coronary artery tone or small platelet clots occurring in the vicinity of an atherosclerotic plaque.In most cases,formation of labile nonocclusive thrombi at the site of a fissured or ulcerated plaque is the mechanism for reduction in flow.The course and the prognosis of unstable angina are variable,but this subset of acute coronary syndrome is associated with a high risk of myocardial infarction and death. PATHOPHYSIOLOGY OF ANGINA Determinants of Myocardial Oxygen Demand As a consequence of its continuous activity,the heart's oxygen needs are relatively high,and it extracts approximately 75%of the available oxygen even in the absence of stress.The myocardial oxygen requirement increases when there is an increase in heart rate,contractility,arterial pressure,or ventricular volume.These hemodynamic alterations frequently occur during physical exercise and sympathetic discharge, which often precipitate angina in patients with obstructive coronary artery disease. The heart favors fatty acids as a substrate for energy production.However,oxidation of fatty acids requires more oxygen per unit of ATP generated than oxidation of carbohydrates.Therefore,drugs that shift myocardial metabolism toward greater use of glucose(fatty acid oxidation inhibitors)have the potential of reducing the oxygen demand without altering hemodynamics. Determinants of Coronary Blood Flow Myocardial Oxygen Supply Increased myocardial demands for oxygen in the normal heart are met by augmenting coronary blood flow.Coronary blood flow is directly related to the perfusion pressure (aortic diastolic pressure)and the duration of diastole.Because coronary flow drops to negligible values during systole,the duration of diastole becomes a limiting factor for myocardial perfusion during tachycardia.Coronary blood flow is inversely proportional to coronary vascular bed resistance.Resistance is determined mainly by intrinsic factors including metabolic products and autonomic activity and by various pharmacologic agents.Damage to the endothelium of coronary vessels has been shown to alter their ability to dilate and to increase coronary vascular resistance. Determinants of Vascular Tone Arteriolar and venous tone (smooth muscle tension)both play a role in determining myocardial wall stress.Arteriolar tone directly controls peripheral vascular resistance and thus arterial blood pressure.In systole,intraventricular pressure must exceed 2
2 Unstable angina, an acute coronary syndrome, is said to be present when there are episodes of angina at rest and when there is a change in the character, frequency, and duration of chest pain as well as precipitating factors in patients with previously stable angina. Unstable angina is caused by episodes of increased epicardial coronary artery tone or small platelet clots occurring in the vicinity of an atherosclerotic plaque. In most cases, formation of labile nonocclusive thrombi at the site of a fissured or ulcerated plaque is the mechanism for reduction in flow. The course and the prognosis of unstable angina are variable, but this subset of acute coronary syndrome is associated with a high risk of myocardial infarction and death. PATHOPHYSIOLOGY OF ANGINA Determinants of Myocardial Oxygen Demand As a consequence of its continuous activity, the heart's oxygen needs are relatively high, and it extracts approximately 75% of the available oxygen even in the absence of stress. The myocardial oxygen requirement increases when there is an increase in heart rate, contractility, arterial pressure, or ventricular volume. These hemodynamic alterations frequently occur during physical exercise and sympathetic discharge, which often precipitate angina in patients with obstructive coronary artery disease. The heart favors fatty acids as a substrate for energy production. However, oxidation of fatty acids requires more oxygen per unit of ATP generated than oxidation of carbohydrates. Therefore, drugs that shift myocardial metabolism toward greater use of glucose (fatty acid oxidation inhibitors) have the potential of reducing the oxygen demand without altering hemodynamics. Determinants of Coronary Blood Flow Myocardial Oxygen Supply Increased myocardial demands for oxygen in the normal heart are met by augmenting coronary blood flow. Coronary blood flow is directly related to the perfusion pressure (aortic diastolic pressure) and the duration of diastole. Because coronary flow drops to negligible values during systole, the duration of diastole becomes a limiting factor for myocardial perfusion during tachycardia. Coronary blood flow is inversely proportional to coronary vascular bed resistance. Resistance is determined mainly by intrinsic factors including metabolic products and autonomic activity and by various pharmacologic agents. Damage to the endothelium of coronary vessels has been shown to alter their ability to dilate and to increase coronary vascular resistance. Determinants of Vascular Tone Arteriolar and venous tone (smooth muscle tension) both play a role in determining myocardial wall stress. Arteriolar tone directly controls peripheral vascular resistance and thus arterial blood pressure. In systole, intraventricular pressure must exceed
aortic pressure to eject blood;arterial blood pressure thus determines the systolic wall stress in an important way.Venous tone determines the capacity of the venous circulation and controls the amount of blood sequestered in the venous system versus the amount returned to the heart.Venous tone thereby determines the diastolic wall stress. The regulation of smooth muscle contraction and relaxation is shown schematically in Figure 1.As shown in Figures 1 and 2,drugs may relax vascular smooth muscle in several ways: (1)Increasing cGMP:As indicated in Figure 2,cGMP facilitates the dephosphorylation of myosin light chains,preventing the interaction of myosin with actin.Nitric oxide is an effective activator of soluble guanylyl cyclase and acts mainly through this mechanism.Important molecular donors of nitric oxide include nitroprusside and the organic nitrates used in angina. (2)Decreasing intracellular Ca:Calcium channel blockers predictably cause vasodilation because they reduce intracellular Ca2,a major modulator of the activation of myosin light chain kinase.(Beta blockers and calcium channel blockers reduce Ca2 influx in cardiac muscle,thereby reducing rate,contractility,and oxygen requirement unless reversed by compensatory responses.) (3)Stabilizing or preventing depolarization of the vascular smooth muscle cell membrane:The membrane potential of excitable cells is stabilized near the resting potential by increasing potassium permeability.Potassium channel openers,such as minoxidil sulfate,increase the permeability of K channels,probably ATP-dependent K*channels.Certain newer agents under investigation for use in angina (eg, nicorandil)may act,in part,by this mechanism. (4)Increasing cAMP in vascular smooth muscle cells:As shown in Figure 1,an increase in cAMP increases the rate of inactivation of myosin light chain kinase,the enzyme responsible for triggering the interaction of actin with myosin in these cells. This appears to be the mechanism of vasodilation caused by 2 agonists,drugs that are not used in angina. 3
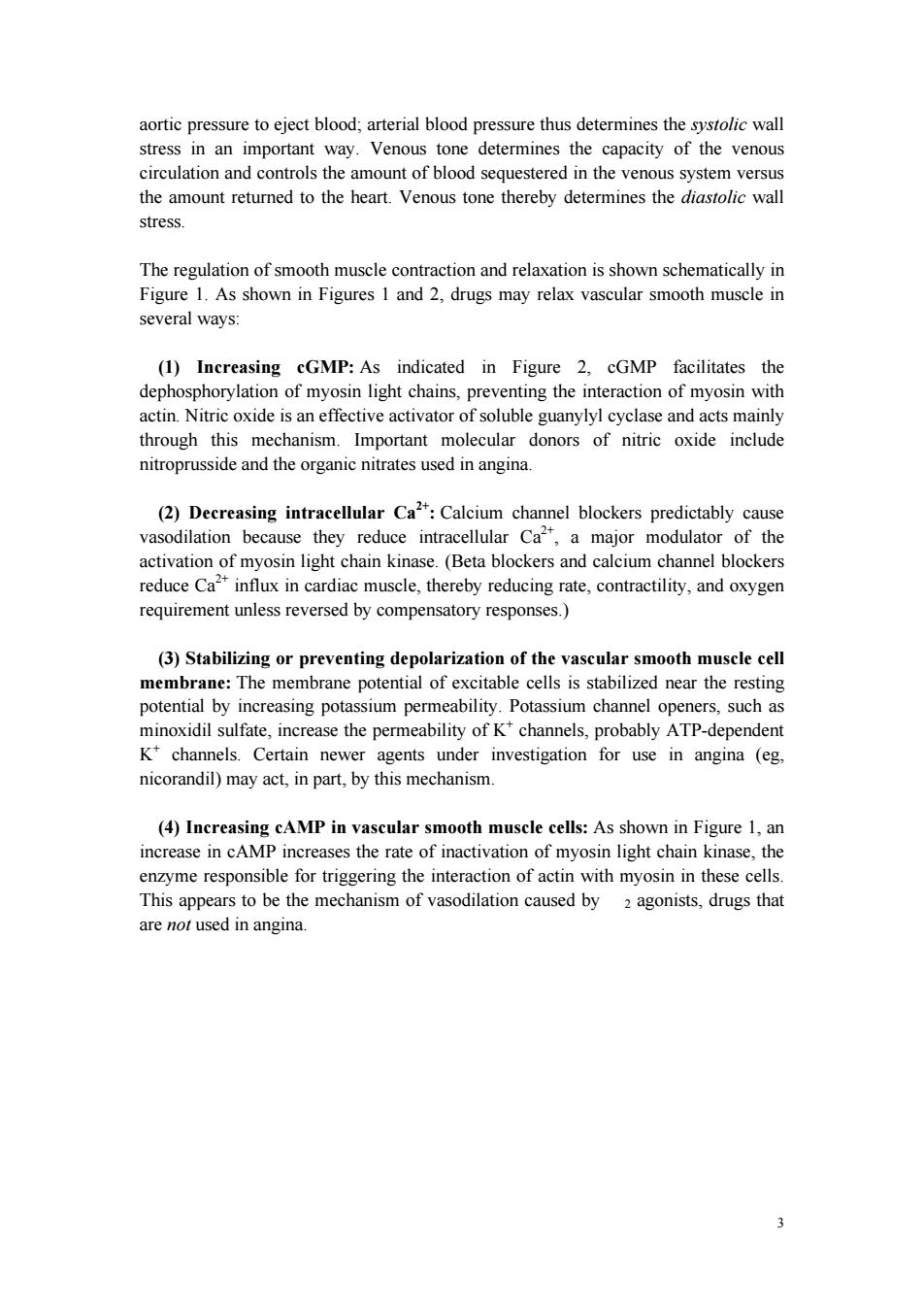
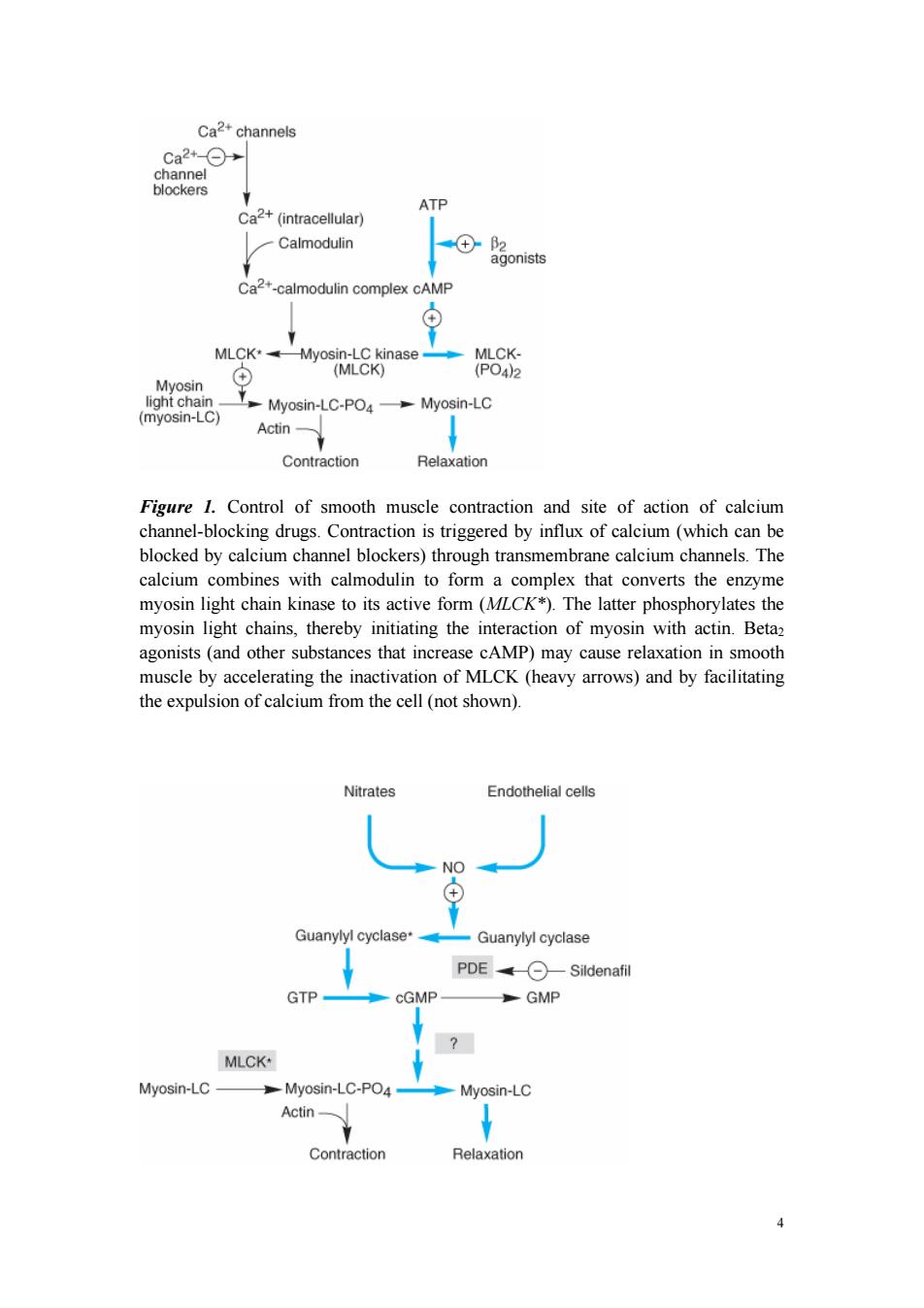
3 aortic pressure to eject blood; arterial blood pressure thus determines the systolic wall stress in an important way. Venous tone determines the capacity of the venous circulation and controls the amount of blood sequestered in the venous system versus the amount returned to the heart. Venous tone thereby determines the diastolic wall stress. The regulation of smooth muscle contraction and relaxation is shown schematically in Figure 1. As shown in Figures 1 and 2, drugs may relax vascular smooth muscle in several ways: (1) Increasing cGMP: As indicated in Figure 2, cGMP facilitates the dephosphorylation of myosin light chains, preventing the interaction of myosin with actin. Nitric oxide is an effective activator of soluble guanylyl cyclase and acts mainly through this mechanism. Important molecular donors of nitric oxide include nitroprusside and the organic nitrates used in angina. (2) Decreasing intracellular Ca2+: Calcium channel blockers predictably cause vasodilation because they reduce intracellular Ca2+, a major modulator of the activation of myosin light chain kinase. (Beta blockers and calcium channel blockers reduce Ca2+ influx in cardiac muscle, thereby reducing rate, contractility, and oxygen requirement unless reversed by compensatory responses.) (3) Stabilizing or preventing depolarization of the vascular smooth muscle cell membrane: The membrane potential of excitable cells is stabilized near the resting potential by increasing potassium permeability. Potassium channel openers, such as minoxidil sulfate, increase the permeability of K+ channels, probably ATP-dependent K+ channels. Certain newer agents under investigation for use in angina (eg, nicorandil) may act, in part, by this mechanism. (4) Increasing cAMP in vascular smooth muscle cells: As shown in Figure 1, an increase in cAMP increases the rate of inactivation of myosin light chain kinase, the enzyme responsible for triggering the interaction of actin with myosin in these cells. This appears to be the mechanism of vasodilation caused by 2 agonists, drugs that are not used in angina
Ca2+channels ca2+-O→ channel blockers ATP Ca2+(intracellular) Calmodulin +-2 agonists Ca2+-calmodulin complex cAMP MLCK*Myosin-LC kinase MLCK- (+ (MLCK) (PO42 Myosin light chain- (myosin-LC) Myosin-LC-PO4Myosin-LC Actin- Contraction Relaxation Figure 1.Control of smooth muscle contraction and site of action of calcium channel-blocking drugs.Contraction is triggered by influx of calcium (which can be blocked by calcium channel blockers)through transmembrane calcium channels.The calcium combines with calmodulin to form a complex that converts the enzyme myosin light chain kinase to its active form (MLCK*).The latter phosphorylates the myosin light chains,thereby initiating the interaction of myosin with actin.Betaz agonists (and other substances that increase cAMP)may cause relaxation in smooth muscle by accelerating the inactivation of MLCK (heavy arrows)and by facilitating the expulsion of calcium from the cell(not shown). Nitrates Endothelial cells NO Guanylyl cyclase* Guanylyl cyclase PDE Sildenafil GTP cGMP GMP MLCK* Myosin-LC Myosin-LC-PO4- Myosin-LC Actin- Contraction Relaxation
4 Figure 1. Control of smooth muscle contraction and site of action of calcium channel-blocking drugs. Contraction is triggered by influx of calcium (which can be blocked by calcium channel blockers) through transmembrane calcium channels. The calcium combines with calmodulin to form a complex that converts the enzyme myosin light chain kinase to its active form (MLCK*). The latter phosphorylates the myosin light chains, thereby initiating the interaction of myosin with actin. Beta2 agonists (and other substances that increase cAMP) may cause relaxation in smooth muscle by accelerating the inactivation of MLCK (heavy arrows) and by facilitating the expulsion of calcium from the cell (not shown)
Figure 2.Mechanism of action of nitrates,nitrites,and other substances that increase the concentration of nitric oxide (NO)in smooth muscle cells.(MLCK*,activated myosin light chain kinase [see Figure 1];guanylyl cyclase*,activated guanylyl cyclase;?unknown intermediate steps.Steps leading to relaxation are shown with heavy arrows. I.BASIC PHARMACOLOGY OF DRUGS USED TO TREAT ANGINA Drug Action in Angina Three of the four drug groups currently approved for use in angina(organic nitrates, calcium channel blockers,and blockers)decrease myocardial oxygen requirement by decreasing the determinants of oxygen demand (heart rate,ventricular volume, blood pressure,and contractility).In some patients,a redistribution of coronary flow may increase oxygen delivery to ischemic tissue.In variant angina,the nitrates and the calcium channel blockers may also increase myocardial oxygen delivery by reversing coronary arterial spasm.The fourth group,represented by ranolazine,is discussed later. NITRATES NITRITES Chemistry These agents are simple nitric and nitrous acid esters of polyalcohols.Nitroglycerin may be considered the prototype of the group.Although nitroglycerin is used in the manufacture of dynamite,the formulations used in medicine are not explosive.The conventional sublingual tablet form of nitroglycerin may lose potency when stored as a result of volatilization and adsorption to plastic surfaces.Therefore,it should be kept in tightly closed glass containers.It is not sensitive to light. All therapeutically active agents in the nitrate group have identical mechanisms of action and similar toxicities.Therefore,pharmacokinetic factors govern the choice of agent and mode of therapy when using the nitrates. Pharmacokinetics The liver contains a high-capacity organic nitrate reductase that removes nitrate groups in a stepwise fashion from the parent molecule and ultimately inactivates the drug.Therefore,oral bioavailability of the traditional organic nitrates (eg, nitroglycerin and isosorbide dinitrate)is very low (typically 10-20%).For this 5
5 Figure 2. Mechanism of action of nitrates, nitrites, and other substances that increase the concentration of nitric oxide (NO) in smooth muscle cells. (MLCK*, activated myosin light chain kinase [see Figure 1]; guanylyl cyclase*, activated guanylyl cyclase; ?, unknown intermediate steps. Steps leading to relaxation are shown with heavy arrows.) I. BASIC PHARMACOLOGY OF DRUGS USED TO TREAT ANGINA Drug Action in Angina Three of the four drug groups currently approved for use in angina (organic nitrates, calcium channel blockers, and blockers) decrease myocardial oxygen requirement by decreasing the determinants of oxygen demand (heart rate, ventricular volume, blood pressure, and contractility). In some patients, a redistribution of coronary flow may increase oxygen delivery to ischemic tissue. In variant angina, the nitrates and the calcium channel blockers may also increase myocardial oxygen delivery by reversing coronary arterial spasm. The fourth group, represented by ranolazine, is discussed later. NITRATES NITRITES Chemistry These agents are simple nitric and nitrous acid esters of polyalcohols. Nitroglycerin may be considered the prototype of the group. Although nitroglycerin is used in the manufacture of dynamite, the formulations used in medicine are not explosive. The conventional sublingual tablet form of nitroglycerin may lose potency when stored as a result of volatilization and adsorption to plastic surfaces. Therefore, it should be kept in tightly closed glass containers. It is not sensitive to light. All therapeutically active agents in the nitrate group have identical mechanisms of action and similar toxicities. Therefore, pharmacokinetic factors govern the choice of agent and mode of therapy when using the nitrates. Pharmacokinetics The liver contains a high-capacity organic nitrate reductase that removes nitrate groups in a stepwise fashion from the parent molecule and ultimately inactivates the drug. Therefore, oral bioavailability of the traditional organic nitrates (eg, nitroglycerin and isosorbide dinitrate) is very low (typically 10-20%). For this