receptors to initiate reflex bronchoconstriction or to release tachykinins(eg,substance P)that directly stimulate smooth muscle contraction. I.BASIC PHARMACOLOGY OF AGENTS USED IN THE TREATMENT OF ASTHMA INTRODUCTION The drugs most used for management of asthma are adrenoceptor agonists,or sympathomimetic agents (used as "relievers"or bronchodilators)and inhaled corticosteroids (used as "controllers"or anti-inflammatory agents).Their basic pharmacology is presented elsewhere.In this chapter,we review their pharmacology relevant to asthma. SYMPATHOMIMETIC AGENTS Introduction The adrenoceptor agonists have several pharmacologic actions that are important in the treatment of asthma.They relax airway smooth muscle and inhibit release of bronchoconstricting mediators from mast cells.They may also inhibit microvascular leakage and increase mucociliary transport by increasing ciliary activity.As in other tissues,the agonists stimulate adenylyl cyclase and increase the formation of intracellular cAMP(Figure 3) The best-characterized action of the adrenoceptor agonists in the airways is relaxation of airway smooth muscle.Although there is no evidence for significant sympathetic innervation of human airway smooth muscle,ample evidence exists for the presence of adrenoceptors on airway smooth muscle.In general,stimulation of 2 receptors relaxes airway smooth muscle,inhibits mediator release,and causes tachycardia and skeletal muscle tremor as side effects. The sympathomimetic agents that have been widely used in the treatment of asthma include epinephrine,ephedrine,isoproterenol,and albuterol and other 2-selective agents(Figure 4).Because epinephrine and isoproterenol increase the rate and force of cardiac contraction (mediated mainly by receptors),they are reserved for special situations(see below). In general,adrenoceptor agonists are best delivered by inhalation because this results in the greatest local effect on airway smooth muscle with the least systemic toxicity. Aerosol deposition depends on the particle size,the pattern of breathing(tidal volume and rate of airflow),and the geometry of the airways.Even with particles in the optimal size range of 2-5 mm,80-90%of the total dose of aerosol is deposited in the
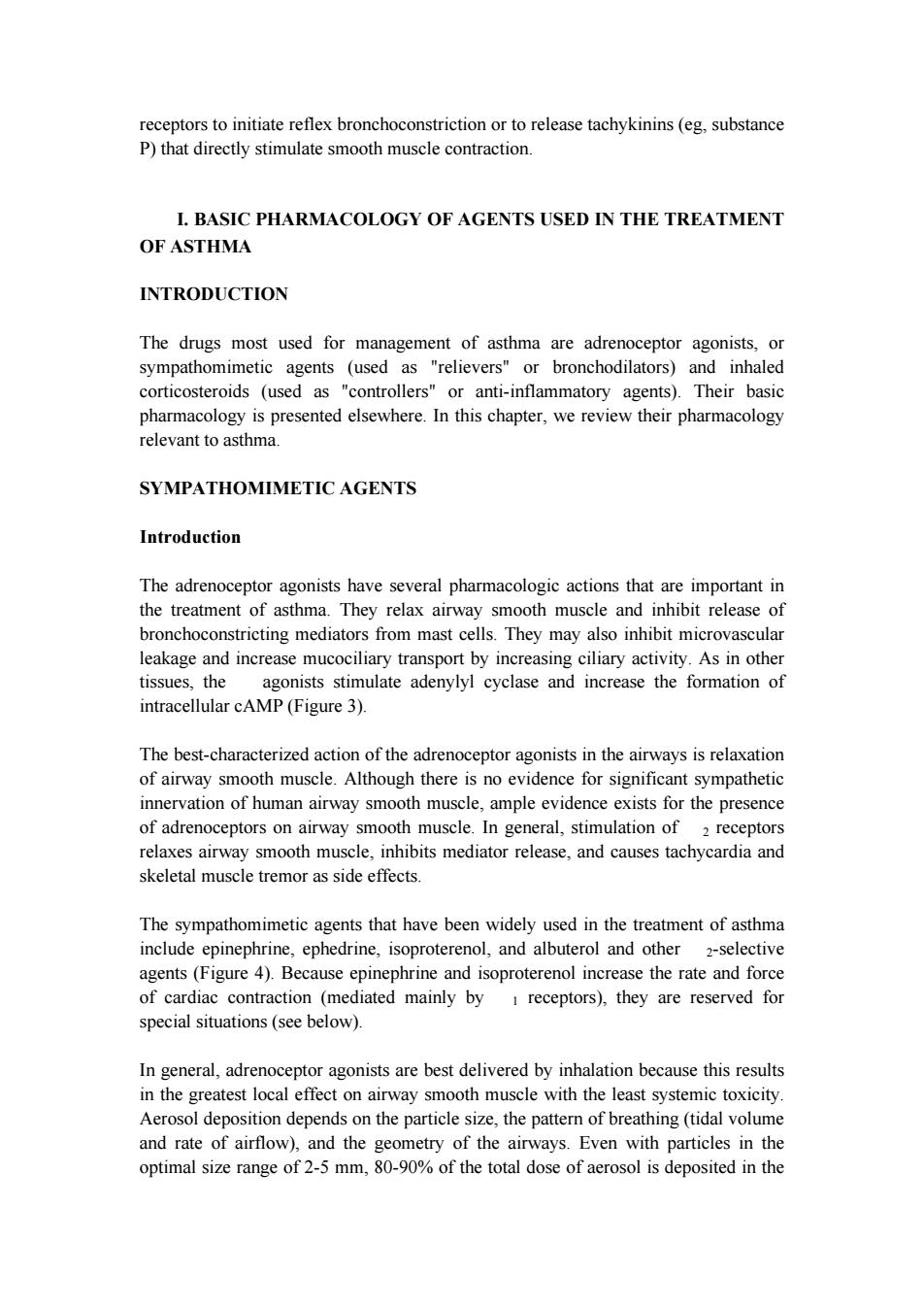
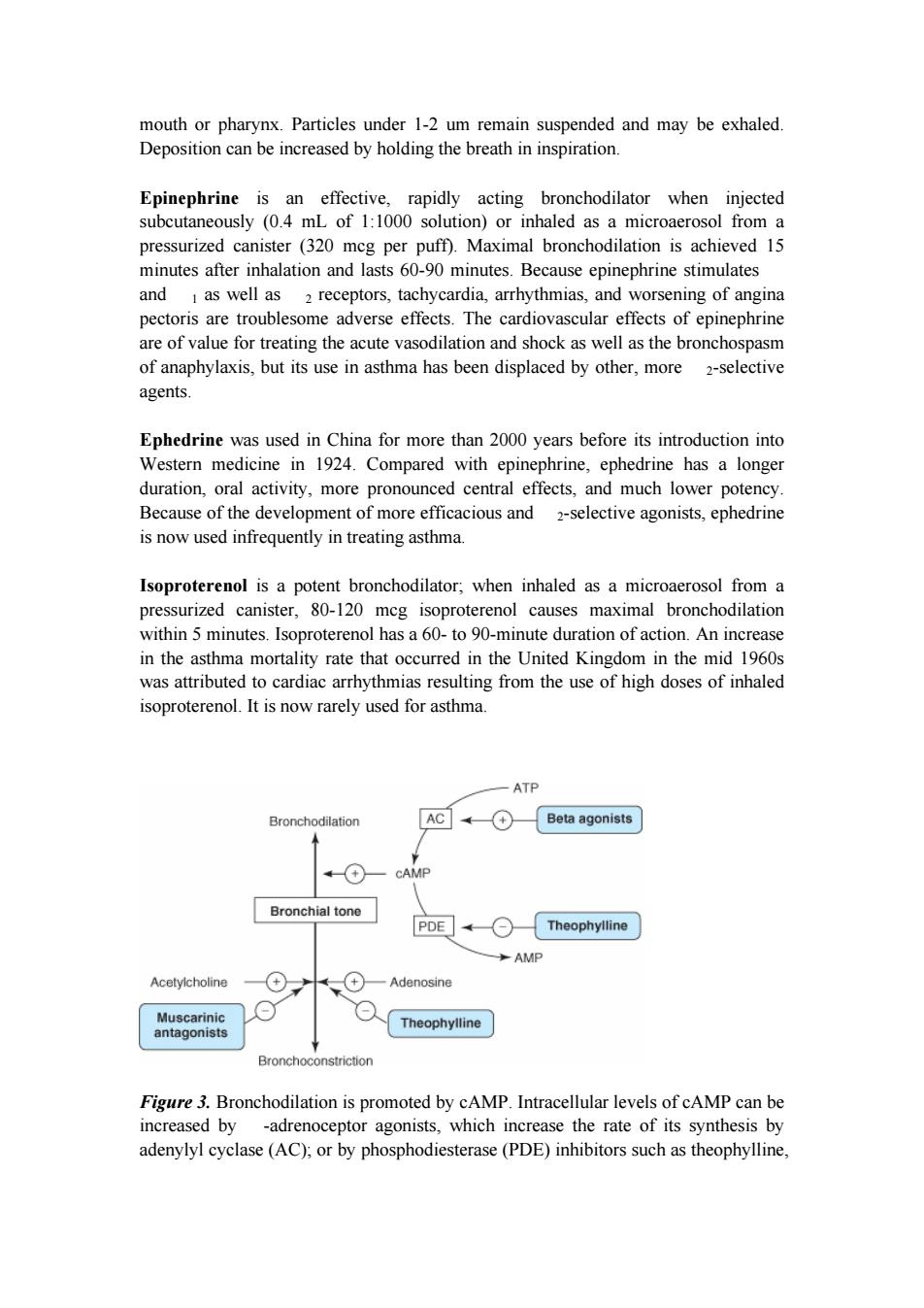
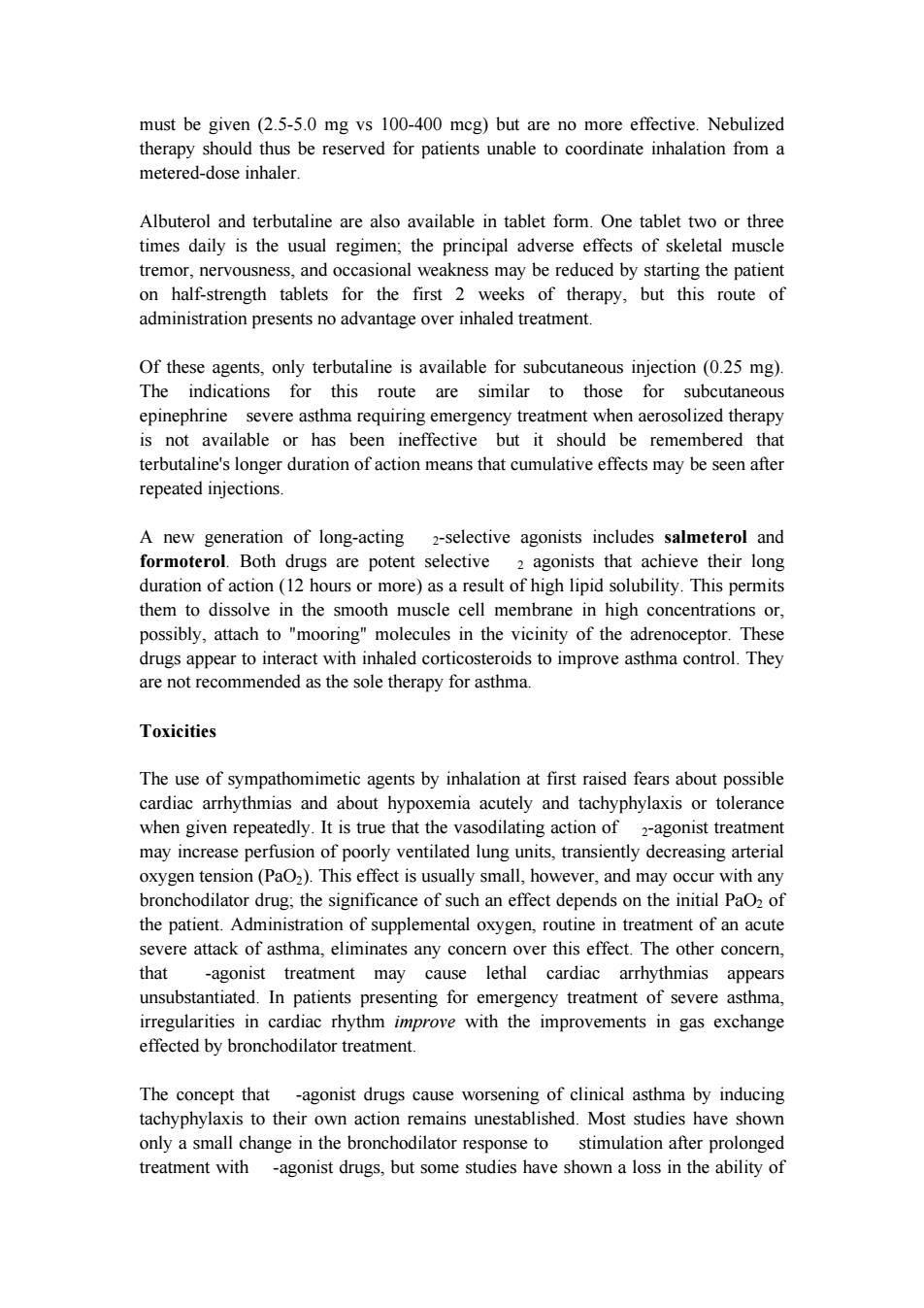
receptors to initiate reflex bronchoconstriction or to release tachykinins (eg, substance P) that directly stimulate smooth muscle contraction. I. BASIC PHARMACOLOGY OF AGENTS USED IN THE TREATMENT OF ASTHMA INTRODUCTION The drugs most used for management of asthma are adrenoceptor agonists, or sympathomimetic agents (used as "relievers" or bronchodilators) and inhaled corticosteroids (used as "controllers" or anti-inflammatory agents). Their basic pharmacology is presented elsewhere. In this chapter, we review their pharmacology relevant to asthma. SYMPATHOMIMETIC AGENTS Introduction The adrenoceptor agonists have several pharmacologic actions that are important in the treatment of asthma. They relax airway smooth muscle and inhibit release of bronchoconstricting mediators from mast cells. They may also inhibit microvascular leakage and increase mucociliary transport by increasing ciliary activity. As in other tissues, the agonists stimulate adenylyl cyclase and increase the formation of intracellular cAMP (Figure 3). The best-characterized action of the adrenoceptor agonists in the airways is relaxation of airway smooth muscle. Although there is no evidence for significant sympathetic innervation of human airway smooth muscle, ample evidence exists for the presence of adrenoceptors on airway smooth muscle. In general, stimulation of 2 receptors relaxes airway smooth muscle, inhibits mediator release, and causes tachycardia and skeletal muscle tremor as side effects. The sympathomimetic agents that have been widely used in the treatment of asthma include epinephrine, ephedrine, isoproterenol, and albuterol and other 2-selective agents (Figure 4). Because epinephrine and isoproterenol increase the rate and force of cardiac contraction (mediated mainly by 1 receptors), they are reserved for special situations (see below). In general, adrenoceptor agonists are best delivered by inhalation because this results in the greatest local effect on airway smooth muscle with the least systemic toxicity. Aerosol deposition depends on the particle size, the pattern of breathing (tidal volume and rate of airflow), and the geometry of the airways. Even with particles in the optimal size range of 2-5 mm, 80-90% of the total dose of aerosol is deposited in the
mouth or pharynx.Particles under 1-2 um remain suspended and may be exhaled. Deposition can be increased by holding the breath in inspiration. Epinephrine is an effective,rapidly acting bronchodilator when injected subcutaneously (0.4 mL of 1:1000 solution)or inhaled as a microaerosol from a pressurized canister (320 mcg per puff).Maximal bronchodilation is achieved 15 minutes after inhalation and lasts 60-90 minutes.Because epinephrine stimulates and I as well as 2 receptors,tachycardia,arrhythmias,and worsening of angina pectoris are troublesome adverse effects.The cardiovascular effects of epinephrine are of value for treating the acute vasodilation and shock as well as the bronchospasm of anaphylaxis,but its use in asthma has been displaced by other,more 2-selective agents. Ephedrine was used in China for more than 2000 years before its introduction into Western medicine in 1924.Compared with epinephrine,ephedrine has a longer duration,oral activity,more pronounced central effects,and much lower potency. Because of the development of more efficacious and 2-selective agonists,ephedrine is now used infrequently in treating asthma. Isoproterenol is a potent bronchodilator;when inhaled as a microaerosol from a pressurized canister,80-120 mcg isoproterenol causes maximal bronchodilation within 5 minutes.Isoproterenol has a 60-to 90-minute duration of action.An increase in the asthma mortality rate that occurred in the United Kingdom in the mid 1960s was attributed to cardiac arrhythmias resulting from the use of high doses of inhaled isoproterenol.It is now rarely used for asthma. ATP Bronchodilation AC (+ Beta agonists A + CAMP Bronchial tone PDE Theophylline AMP Acetylcholine Adenosine Muscarinic Theophylline antagonists Bronchoconstriction Figure 3.Bronchodilation is promoted by cAMP.Intracellular levels of cAMP can be increased by -adrenoceptor agonists,which increase the rate of its synthesis by adenylyl cyclase(AC);or by phosphodiesterase(PDE)inhibitors such as theophylline
mouth or pharynx. Particles under 1-2 um remain suspended and may be exhaled. Deposition can be increased by holding the breath in inspiration. Epinephrine is an effective, rapidly acting bronchodilator when injected subcutaneously (0.4 mL of 1:1000 solution) or inhaled as a microaerosol from a pressurized canister (320 mcg per puff). Maximal bronchodilation is achieved 15 minutes after inhalation and lasts 60-90 minutes. Because epinephrine stimulates and 1 as well as 2 receptors, tachycardia, arrhythmias, and worsening of angina pectoris are troublesome adverse effects. The cardiovascular effects of epinephrine are of value for treating the acute vasodilation and shock as well as the bronchospasm of anaphylaxis, but its use in asthma has been displaced by other, more 2-selective agents. Ephedrine was used in China for more than 2000 years before its introduction into Western medicine in 1924. Compared with epinephrine, ephedrine has a longer duration, oral activity, more pronounced central effects, and much lower potency. Because of the development of more efficacious and 2-selective agonists, ephedrine is now used infrequently in treating asthma. Isoproterenol is a potent bronchodilator; when inhaled as a microaerosol from a pressurized canister, 80-120 mcg isoproterenol causes maximal bronchodilation within 5 minutes. Isoproterenol has a 60- to 90-minute duration of action. An increase in the asthma mortality rate that occurred in the United Kingdom in the mid 1960s was attributed to cardiac arrhythmias resulting from the use of high doses of inhaled isoproterenol. It is now rarely used for asthma. Figure 3. Bronchodilation is promoted by cAMP. Intracellular levels of cAMP can be increased by -adrenoceptor agonists, which increase the rate of its synthesis by adenylyl cyclase (AC); or by phosphodiesterase (PDE) inhibitors such as theophylline
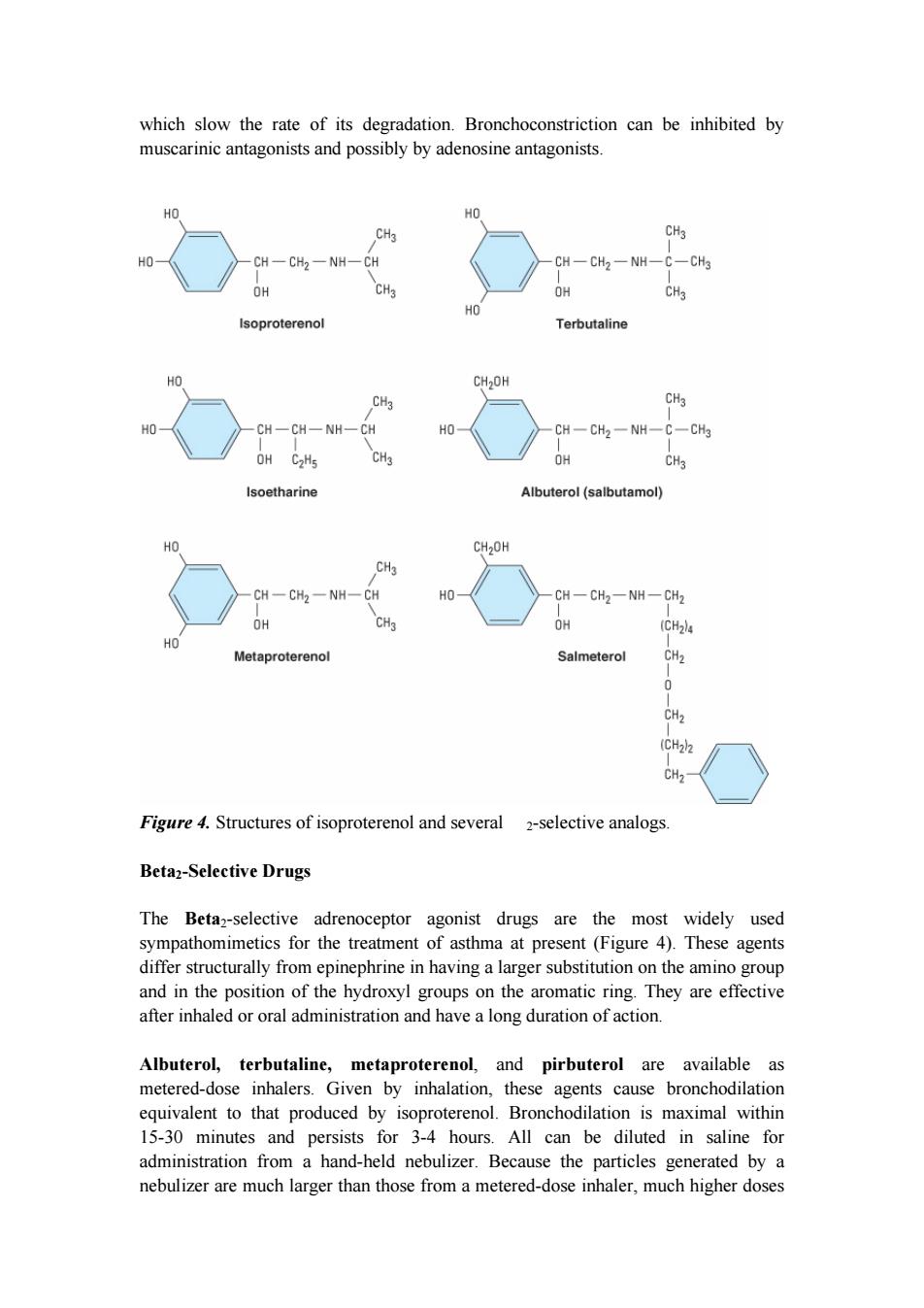
which slow the rate of its degradation.Bronchoconstriction can be inhibited by muscarinic antagonists and possibly by adenosine antagonists. HO HO CH3 CH3 CH一CH2一NH-CH CH-CH2-NH-C-CH3 OH CH3 OH CH3 HO Isoproterenol Terbutaline HO CH2OH CH3 CH3 HO CH-CH一NH-CH HO CH-CH2一NH-C-CH3 OH C2H5 CH3 OH CH3 Isoetharine Albuterol(salbutamol) HO CH2OH CH3 CH-CH2-NH-CH HO CH一CH2-NH-CH2 OH CH3 OH (CH24 HO Metaproterenol Salmeterol CH2 0 CH2 (CH22 CH2 Figure 4.Structures of isoproterenol and several 2-selective analogs. Beta2-Selective Drugs The Beta2-selective adrenoceptor agonist drugs are the most widely used sympathomimetics for the treatment of asthma at present(Figure 4).These agents differ structurally from epinephrine in having a larger substitution on the amino group and in the position of the hydroxyl groups on the aromatic ring.They are effective after inhaled or oral administration and have a long duration of action. Albuterol,terbutaline,metaproterenol,and pirbuterol are available as metered-dose inhalers.Given by inhalation,these agents cause bronchodilation equivalent to that produced by isoproterenol.Bronchodilation is maximal within 15-30 minutes and persists for 3-4 hours.All can be diluted in saline for administration from a hand-held nebulizer.Because the particles generated by a nebulizer are much larger than those from a metered-dose inhaler,much higher doses
which slow the rate of its degradation. Bronchoconstriction can be inhibited by muscarinic antagonists and possibly by adenosine antagonists. Figure 4. Structures of isoproterenol and several 2-selective analogs. Beta2-Selective Drugs The Beta2-selective adrenoceptor agonist drugs are the most widely used sympathomimetics for the treatment of asthma at present (Figure 4). These agents differ structurally from epinephrine in having a larger substitution on the amino group and in the position of the hydroxyl groups on the aromatic ring. They are effective after inhaled or oral administration and have a long duration of action. Albuterol, terbutaline, metaproterenol, and pirbuterol are available as metered-dose inhalers. Given by inhalation, these agents cause bronchodilation equivalent to that produced by isoproterenol. Bronchodilation is maximal within 15-30 minutes and persists for 3-4 hours. All can be diluted in saline for administration from a hand-held nebulizer. Because the particles generated by a nebulizer are much larger than those from a metered-dose inhaler, much higher doses
must be given(2.5-5.0 mg vs 100-400 mcg)but are no more effective.Nebulized therapy should thus be reserved for patients unable to coordinate inhalation from a metered-dose inhaler. Albuterol and terbutaline are also available in tablet form.One tablet two or three times daily is the usual regimen;the principal adverse effects of skeletal muscle tremor,nervousness,and occasional weakness may be reduced by starting the patient on half-strength tablets for the first 2 weeks of therapy,but this route of administration presents no advantage over inhaled treatment. Of these agents,only terbutaline is available for subcutaneous injection (0.25 mg). The indications for this route are similar to those for subcutaneous epinephrine severe asthma requiring emergency treatment when aerosolized therapy is not available or has been ineffective but it should be remembered that terbutaline's longer duration of action means that cumulative effects may be seen after repeated injections. A new generation of long-acting 2-selective agonists includes salmeterol and formoterol.Both drugs are potent selective 2 agonists that achieve their long duration of action(12 hours or more)as a result of high lipid solubility.This permits them to dissolve in the smooth muscle cell membrane in high concentrations or, possibly,attach to "mooring"molecules in the vicinity of the adrenoceptor.These drugs appear to interact with inhaled corticosteroids to improve asthma control.They are not recommended as the sole therapy for asthma. Toxicities The use of sympathomimetic agents by inhalation at first raised fears about possible cardiac arrhythmias and about hypoxemia acutely and tachyphylaxis or tolerance when given repeatedly.It is true that the vasodilating action of 2-agonist treatment may increase perfusion of poorly ventilated lung units,transiently decreasing arterial oxygen tension(PaO2).This effect is usually small,however,and may occur with any bronchodilator drug;the significance of such an effect depends on the initial PaOz of the patient.Administration of supplemental oxygen,routine in treatment of an acute severe attack of asthma,eliminates any concern over this effect.The other concern, that -agonist treatment may cause lethal cardiac arrhythmias appears unsubstantiated.In patients presenting for emergency treatment of severe asthma, irregularities in cardiac rhythm improve with the improvements in gas exchange effected by bronchodilator treatment. The concept that -agonist drugs cause worsening of clinical asthma by inducing tachyphylaxis to their own action remains unestablished.Most studies have shown only a small change in the bronchodilator response to stimulation after prolonged treatment with -agonist drugs,but some studies have shown a loss in the ability of
must be given (2.5-5.0 mg vs 100-400 mcg) but are no more effective. Nebulized therapy should thus be reserved for patients unable to coordinate inhalation from a metered-dose inhaler. Albuterol and terbutaline are also available in tablet form. One tablet two or three times daily is the usual regimen; the principal adverse effects of skeletal muscle tremor, nervousness, and occasional weakness may be reduced by starting the patient on half-strength tablets for the first 2 weeks of therapy, but this route of administration presents no advantage over inhaled treatment. Of these agents, only terbutaline is available for subcutaneous injection (0.25 mg). The indications for this route are similar to those for subcutaneous epinephrine severe asthma requiring emergency treatment when aerosolized therapy is not available or has been ineffective but it should be remembered that terbutaline's longer duration of action means that cumulative effects may be seen after repeated injections. A new generation of long-acting 2-selective agonists includes salmeterol and formoterol. Both drugs are potent selective 2 agonists that achieve their long duration of action (12 hours or more) as a result of high lipid solubility. This permits them to dissolve in the smooth muscle cell membrane in high concentrations or, possibly, attach to "mooring" molecules in the vicinity of the adrenoceptor. These drugs appear to interact with inhaled corticosteroids to improve asthma control. They are not recommended as the sole therapy for asthma. Toxicities The use of sympathomimetic agents by inhalation at first raised fears about possible cardiac arrhythmias and about hypoxemia acutely and tachyphylaxis or tolerance when given repeatedly. It is true that the vasodilating action of 2-agonist treatment may increase perfusion of poorly ventilated lung units, transiently decreasing arterial oxygen tension (PaO2). This effect is usually small, however, and may occur with any bronchodilator drug; the significance of such an effect depends on the initial PaO2 of the patient. Administration of supplemental oxygen, routine in treatment of an acute severe attack of asthma, eliminates any concern over this effect. The other concern, that -agonist treatment may cause lethal cardiac arrhythmias appears unsubstantiated. In patients presenting for emergency treatment of severe asthma, irregularities in cardiac rhythm improve with the improvements in gas exchange effected by bronchodilator treatment. The concept that -agonist drugs cause worsening of clinical asthma by inducing tachyphylaxis to their own action remains unestablished. Most studies have shown only a small change in the bronchodilator response to stimulation after prolonged treatment with -agonist drugs, but some studies have shown a loss in the ability of

-agonist treatment to inhibit the response to subsequent challenge with exercise, methacholine,or antigen challenge (referred to as a loss of bronchoprotective action). Fears that heavy use of -agonist inhalers could actually increase morbidity and mortality have not been borne out by careful epidemiologic investigations.Heavy use most often indicates that the patient should be receiving more effective prophylactic therapy with corticosteroids. Although it is true that 2-adrenoceptor agonists appear to be safe and effective bronchodilators for most patients,there is some evidence that the risk of adverse effects from chronic treatment with long-acting agonists may be greater for some individuals,possibly as a function of genetic variants for the receptor.Two retrospective and one prospective study have shown differences between patients homozygous for glycine versus arginine at the B-16 locus of the receptor.Among patients homozygous for arginine,a genotype found in 16%of the Caucasian population in the USA,but more commonly in African Americans,asthma control deteriorated with regular use of albuterol or salmeterol,whereas asthma control improved with this treatment among those homozygous for glycine at the same locus. These findings need to be replicated in larger studies,but it is tempting to speculate that a genetic variant may underlie the report of an increase in asthma mortality from regular use of a long-acting agonist in studies involving very large numbers of patients METHYLXANTHINE DRUGS Introduction The three important methylxanthines are theophylline,theobromine,and caffeine. Their major source is beverages(tea,cocoa,and coffee,respectively).The importance of theophylline as a therapeutic agent in the treatment of asthma has waned as the greater effectiveness of inhaled adrenoceptor agents for acute asthma and of inhaled anti-inflammatory agents for chronic asthma has been established,but theophylline's very low cost is an important advantage for economically disadvantaged patients in societies in which health care resources are limited. Chemistry As shown below,theophylline is 1,3-dimethylxanthine;theobromine is 3,7-dimethylxanthine;and caffeine is 1,3,7-trimethylxanthine.A theophylline preparation commonly used for therapeutic purposes is aminophylline,a theophylline-ethylenediamine complex.The pharmacokinetics of theophylline are discussed below.The metabolic products,partially demethylated xanthines(not uric acid),are excreted in the urine
-agonist treatment to inhibit the response to subsequent challenge with exercise, methacholine, or antigen challenge (referred to as a loss of bronchoprotective action). Fears that heavy use of -agonist inhalers could actually increase morbidity and mortality have not been borne out by careful epidemiologic investigations. Heavy use most often indicates that the patient should be receiving more effective prophylactic therapy with corticosteroids. Although it is true that 2-adrenoceptor agonists appear to be safe and effective bronchodilators for most patients, there is some evidence that the risk of adverse effects from chronic treatment with long-acting agonists may be greater for some individuals, possibly as a function of genetic variants for the receptor. Two retrospective and one prospective study have shown differences between patients homozygous for glycine versus arginine at the B-16 locus of the receptor. Among patients homozygous for arginine, a genotype found in 16% of the Caucasian population in the USA, but more commonly in African Americans, asthma control deteriorated with regular use of albuterol or salmeterol, whereas asthma control improved with this treatment among those homozygous for glycine at the same locus. These findings need to be replicated in larger studies, but it is tempting to speculate that a genetic variant may underlie the report of an increase in asthma mortality from regular use of a long-acting agonist in studies involving very large numbers of patients. METHYLXANTHINE DRUGS Introduction The three important methylxanthines are theophylline, theobromine, and caffeine. Their major source is beverages (tea, cocoa, and coffee, respectively). The importance of theophylline as a therapeutic agent in the treatment of asthma has waned as the greater effectiveness of inhaled adrenoceptor agents for acute asthma and of inhaled anti-inflammatory agents for chronic asthma has been established, but theophylline's very low cost is an important advantage for economically disadvantaged patients in societies in which health care resources are limited. Chemistry As shown below, theophylline is 1,3-dimethylxanthine; theobromine is 3,7-dimethylxanthine; and caffeine is 1,3,7-trimethylxanthine. A theophylline preparation commonly used for therapeutic purposes is aminophylline, a theophylline-ethylenediamine complex. The pharmacokinetics of theophylline are discussed below. The metabolic products, partially demethylated xanthines (not uric acid), are excreted in the urine