
Pharmacokinetics Salicylic acid is a simple organic acid with a pKa of 3.0.Aspirin(acetylsalicylic acid; ASA)has a pKa of 3.5.Sodium salicylate and aspirin (Figure 36-2)are equally effective anti-inflammatory drugs,though aspirin may be more effective as an analgesic.The salicylates are rapidly absorbed from the stomach and upper small intestine,yielding a peak plasma salicylate level within 1-2 hours.Aspirin is absorbed as such and is rapidly hydrolyzed (serum half-life 15 minutes)to acetic acid and salicylate by esterases in tissue and blood.Salicylate is bound to albumin,but the binding and metabolism of salicylates are saturable so that the unbound fraction increases as total concentration increases.Beyond a total body load of 600 mg, increases in salicylate dosage increase salicylate concentration disproportionately.As doses of aspirin increase,salicylate elimination half-life increases from 3-5 hours(for 600 mg/d dosage)to 12-16 hours (dosage 3.6 g/d).Alkalinization of the urine increases the rate of excretion of free salicylate and its water-soluble conjugates. 0-Na CH OH Aspirin 0 Sodium salicylate -0 HO-C-CH3 OH Acetic acid Salicylate Conjugation with Conjugation glucuronic acid Oxidation with glycine H 0 Ester and ether -N-CH2-COOH Free HO -0H glucuronides salicylate OH OH Salicyluric acid Gentisic acid (1%) Figure 36-2.Structure and metabolism of the salicylates.(Modified and reproduced, with permission,from Meyers FH,Jawetz E,Goldfien A:Review of Medical Pharmacology,7th ed.McGraw-Hill,1980.) Mechanisms of Action A.ANTI-INFLAMMATORY EFFECTS Aspirin is a nonselective inhibitor of both COX isoforms(Figure 36-3),but salicylate is much less effective in inhibiting either isoform.Nonacetylated salicylates may work as oxygen radical scavengers.Aspirin irreversibly inhibits COX and inhibits platelet aggregation,while nonacetylated salicylates do not
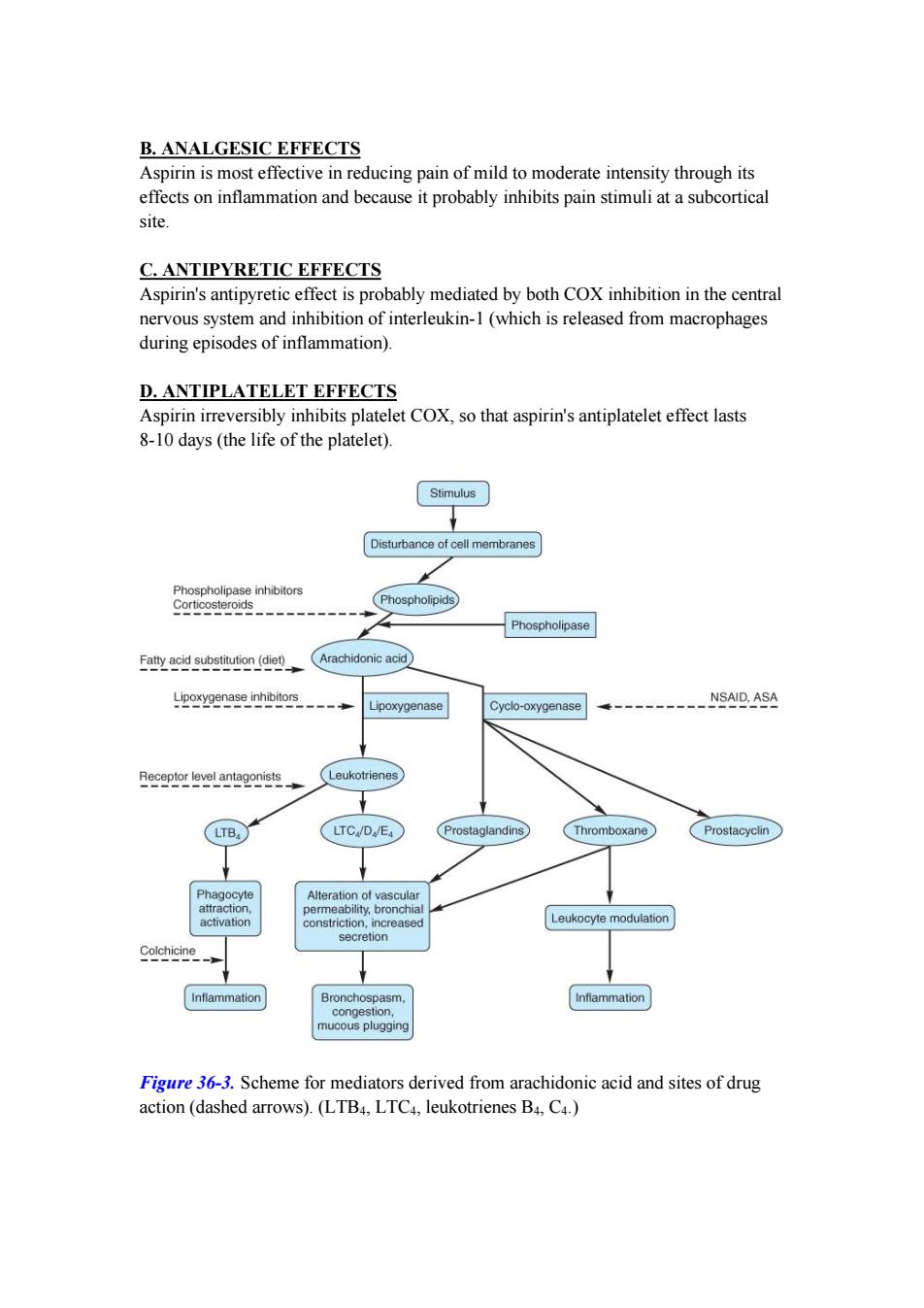
Pharmacokinetics Salicylic acid is a simple organic acid with a pKa of 3.0. Aspirin (acetylsalicylic acid; ASA) has a pKa of 3.5. Sodium salicylate and aspirin (Figure 36-2) are equally effective anti-inflammatory drugs, though aspirin may be more effective as an analgesic. The salicylates are rapidly absorbed from the stomach and upper small intestine, yielding a peak plasma salicylate level within 1-2 hours. Aspirin is absorbed as such and is rapidly hydrolyzed (serum half-life 15 minutes) to acetic acid and salicylate by esterases in tissue and blood. Salicylate is bound to albumin, but the binding and metabolism of salicylates are saturable so that the unbound fraction increases as total concentration increases. Beyond a total body load of 600 mg, increases in salicylate dosage increase salicylate concentration disproportionately. As doses of aspirin increase, salicylate elimination half-life increases from 3-5 hours (for 600 mg/d dosage) to 12-16 hours (dosage > 3.6 g/d). Alkalinization of the urine increases the rate of excretion of free salicylate and its water-soluble conjugates. Figure 36-2. Structure and metabolism of the salicylates. (Modified and reproduced, with permission, from Meyers FH, Jawetz E, Goldfien A: Review of Medical Pharmacology, 7th ed. McGraw-Hill, 1980.) Mechanisms of Action A. ANTI-INFLAMMATORY EFFECTS Aspirin is a nonselective inhibitor of both COX isoforms (Figure 36-3), but salicylate is much less effective in inhibiting either isoform. Nonacetylated salicylates may work as oxygen radical scavengers. Aspirin irreversibly inhibits COX and inhibits platelet aggregation, while nonacetylated salicylates do not
B.ANALGESIC EFFECTS Aspirin is most effective in reducing pain of mild to moderate intensity through its effects on inflammation and because it probably inhibits pain stimuli at a subcortical site. C.ANTIPYRETIC EFFECTS Aspirin's antipyretic effect is probably mediated by both COX inhibition in the central nervous system and inhibition of interleukin-1(which is released from macrophages during episodes of inflammation). D.ANTIPLATELET EFFECTS Aspirin irreversibly inhibits platelet COX,so that aspirin's antiplatelet effect lasts 8-10 days(the life of the platelet). Stimulus Disturbance of cell membranes Phospholipase inhibitors Corticosteroids Phospholipids Phospholipase Fatty acid substitution(diet) Arachidonic acid Lipoxygenase inhibitors NSAID,ASA Lipoxygenase Cyclo-oxygenase Receptor level antagonists Leukotrienes LTB, LTC/D/E4 Prostaglandins Thromboxane Prostacyclin Phagocyte Alteration of vascular attraction, permeability,bronchial activation constriction,increased Leukocyte modulation secretion Colchicine Inflammation Bronchospasm, Inflammation congestion, mucous plugging Figure 36-3.Scheme for mediators derived from arachidonic acid and sites of drug action(dashed arrows).(LTB4,LTC4,leukotrienes B4,C4.)
B. ANALGESIC EFFECTS Aspirin is most effective in reducing pain of mild to moderate intensity through its effects on inflammation and because it probably inhibits pain stimuli at a subcortical site. C. ANTIPYRETIC EFFECTS Aspirin's antipyretic effect is probably mediated by both COX inhibition in the central nervous system and inhibition of interleukin-1 (which is released from macrophages during episodes of inflammation). D. ANTIPLATELET EFFECTS Aspirin irreversibly inhibits platelet COX, so that aspirin's antiplatelet effect lasts 8-10 days (the life of the platelet). Figure 36-3. Scheme for mediators derived from arachidonic acid and sites of drug action (dashed arrows). (LTB4, LTC4, leukotrienes B4, C4.)
Clinical Uses A.ANALGESIA,ANTIPYRESIS,AND ANTI-INFLAMMATORY EFFECTS Aspirin is employed for mild to moderate pain of varied origin but is not effective for severe visceral pain.Aspirin and other NSAIDs have been combined with opioid analgesics for treatment of cancer pain,where their anti-inflammatory effects act synergistically with the opioids to enhance analgesia.High-dose salicylates are effective for treatment of rheumatic fever,rheumatoid arthritis,and other inflammatory joint conditions. B.OTHER EFFECTS Aspirin decreases the incidence of transient ischemic attacks,unstable angina, coronary artery thrombosis with myocardial infarction,and thrombosis after coronary artery bypass grafting(see Chapter 34). Epidemiologic studies suggest that long-term use of aspirin at low dosage is associated with a lower incidence of colon cancer,possibly related to its COX-inhibiting effects. Dosage The optimal analgesic or antipyretic dose of aspirin is less than the 0.6-0.65 g oral dose commonly used.The anti-inflammatory dose for children is 50-75 mg/kg/d in divided doses and the average starting anti-inflammatory dose for adults is 45 mg/kg/d in divided dose. Adverse Effects At the usual dosage,aspirin's main adverse effects are gastric upset (intolerance)and gastric and duodenal ulcers;hepatotoxicity,asthma,rashes,and renal toxicity occur less frequently.A dose-related increase in fecal blood loss is routinely associated with aspirin administration,although some mucosal adaptation occurs in many patients,so that blood loss declines back to baseline over 4-6 weeks. With higher doses,patients may experience salicylismvomiting,tinnitus,decreased hearing,and vertigoreversible by reducing the dosage.Still larger doses of salicylates cause hyperpnea through a direct effect on the medulla.At toxic salicylate levels,respiratory alkalosis followed by metabolic acidosis(salicylate accumulation). respiratory depression,and even cardiotoxicity and glucose intolerance can occur. Like other NSAIDs,aspirin can cause elevation of liver enzymes (a frequent but mild effect),hepatitis(rare),decreased renal function,bleeding,rashes,and asthma. The antiplatelet action of aspirin contraindicates its use by patients with hemophilia. Although previously not recommended during pregnancy,aspirin may be valuable in
Clinical Uses A. ANALGESIA, ANTIPYRESIS, AND ANTI-INFLAMMATORY EFFECTS Aspirin is employed for mild to moderate pain of varied origin but is not effective for severe visceral pain. Aspirin and other NSAIDs have been combined with opioid analgesics for treatment of cancer pain, where their anti-inflammatory effects act synergistically with the opioids to enhance analgesia. High-dose salicylates are effective for treatment of rheumatic fever, rheumatoid arthritis, and other inflammatory joint conditions. B. OTHER EFFECTS Aspirin decreases the incidence of transient ischemic attacks, unstable angina, coronary artery thrombosis with myocardial infarction, and thrombosis after coronary artery bypass grafting (see Chapter 34). Epidemiologic studies suggest that long-term use of aspirin at low dosage is associated with a lower incidence of colon cancer, possibly related to its COX-inhibiting effects. Dosage The optimal analgesic or antipyretic dose of aspirin is less than the 0.6-0.65 g oral dose commonly used. The anti-inflammatory dose for children is 50-75 mg/kg/d in divided doses and the average starting anti-inflammatory dose for adults is 45 mg/kg/d in divided dose. Adverse Effects At the usual dosage, aspirin's main adverse effects are gastric upset (intolerance) and gastric and duodenal ulcers; hepatotoxicity, asthma, rashes, and renal toxicity occur less frequently. A dose-related increase in fecal blood loss is routinely associated with aspirin administration, although some mucosal adaptation occurs in many patients, so that blood loss declines back to baseline over 4-6 weeks. With higher doses, patients may experience salicylism¾vomiting, tinnitus, decreased hearing, and vertigo¾reversible by reducing the dosage. Still larger doses of salicylates cause hyperpnea through a direct effect on the medulla. At toxic salicylate levels, respiratory alkalosis followed by metabolic acidosis (salicylate accumulation), respiratory depression, and even cardiotoxicity and glucose intolerance can occur. Like other NSAIDs, aspirin can cause elevation of liver enzymes (a frequent but mild effect), hepatitis (rare), decreased renal function, bleeding, rashes, and asthma. The antiplatelet action of aspirin contraindicates its use by patients with hemophilia. Although previously not recommended during pregnancy, aspirin may be valuable in

treating preeclampsia-eclampsia Salicylate overdosage constitutes a medical emergency and requires hospitalization. NONACETYLATED SALICYLATES Introduction These drugs include magnesium choline salicylate,sodium salicylate,and salicylsalicylate.All nonacetylated salicylates are effective anti-inflammatory drugs, although they may be less effective analgesics than aspirin.Because they are much less effective than aspirin as COX inhibitors,they may be preferable when COX inhibition is undesirable,such as in patients with asthma,those with bleeding tendencies,and even (under close supervision)those with renal dysfunction. The nonacetylated salicylates are administered in the same dosage as aspirin and can be monitored using serum salicylate measurements. COX-2 Selective Inhibitors COX-2 selective inhibitors,or coxibs,were developed in an attempt to inhibit prostaglandin synthesis by the COX-2 isoenzyme induced at sites of inflammation without affecting the action of the constitutively active "housekeeping"COX-1 isoenzyme found in the gastrointestinal tract,kidneys,and platelets.Coxibs selectively bind to and block the active site of the COX-2 enzyme much more effectively than that of COX-1.COX-2 inhibitors have analgesic,antipyretic,and anti-inflammatory effects similar to those of nonselective NSAIDs but with an approximate halving of gastrointestinal adverse effects.Likewise,COX-2 inhibitors at usual doses have been shown to have no impact on platelet aggregation,which is mediated by the COX-1 isoenzyme.As a result,COX-2 inhibitors do not offer the cardioprotective effects of traditional nonselective NSAIDs,which has resulted in some patients taking low-dose aspirin in addition to a coxib regimen to maintain this effect.Unfortunately,because COX-2 is constitutively active within the kidney, recommended doses of COX-2 inhibitors cause renal toxicities similar to those associated with traditional NSAIDs.Clinical data have suggested a higher incidence of cardiovascular thrombotic events associated with COX-2 inhibitors such as rofecoxib and valdecoxib,resulting in their withdrawal from the market. 1.Celecoxib Celecoxib is a selective COX-2 inhibitorabout 10-20 times more selective for COX-2 than for COX-1
treating preeclampsia-eclampsia. Salicylate overdosage constitutes a medical emergency and requires hospitalization. NONACETYLATED SALICYLATES Introduction These drugs include magnesium choline salicylate, sodium salicylate, and salicylsalicylate. All nonacetylated salicylates are effective anti-inflammatory drugs, although they may be less effective analgesics than aspirin. Because they are much less effective than aspirin as COX inhibitors, they may be preferable when COX inhibition is undesirable, such as in patients with asthma, those with bleeding tendencies, and even (under close supervision) those with renal dysfunction. The nonacetylated salicylates are administered in the same dosage as aspirin and can be monitored using serum salicylate measurements. COX-2 Selective Inhibitors COX-2 selective inhibitors, or coxibs, were developed in an attempt to inhibit prostaglandin synthesis by the COX-2 isoenzyme induced at sites of inflammation without affecting the action of the constitutively active "housekeeping" COX-1 isoenzyme found in the gastrointestinal tract, kidneys, and platelets. Coxibs selectively bind to and block the active site of the COX-2 enzyme much more effectively than that of COX-1. COX-2 inhibitors have analgesic, antipyretic, and anti-inflammatory effects similar to those of nonselective NSAIDs but with an approximate halving of gastrointestinal adverse effects. Likewise, COX-2 inhibitors at usual doses have been shown to have no impact on platelet aggregation, which is mediated by the COX-1 isoenzyme. As a result, COX-2 inhibitors do not offer the cardioprotective effects of traditional nonselective NSAIDs, which has resulted in some patients taking low-dose aspirin in addition to a coxib regimen to maintain this effect. Unfortunately, because COX-2 is constitutively active within the kidney, recommended doses of COX-2 inhibitors cause renal toxicities similar to those associated with traditional NSAIDs. Clinical data have suggested a higher incidence of cardiovascular thrombotic events associated with COX-2 inhibitors such as rofecoxib and valdecoxib, resulting in their withdrawal from the market. 1. Celecoxib Celecoxib is a selective COX-2 inhibitor¾about 10-20 times more selective for COX-2 than for COX-1

Celecoxib is as effective as other NSAIDs in the treatment of rheumatoid arthritis and osteoarthritis,and in trials it has caused fewer endoscopic ulcers than most other NSAIDs.Probably because it is a sulfonamide,celecoxib may cause rashes.It does not affect platelet aggregation at usual doses.It interacts occasionally with warfarin%as would be expected of a drug metabolized via CYP2C9. Although celecoxib is associated with about half the gastrointestinal side effects of nonselective NSAIDs,the frequency of other adverse effects approximates that of other NSAIDs.Celecoxib causes no more edema or renal effects than other members of the NSAID group,but edema and hypertension have been documented. 2.Etoricoxib Etoricoxib,a bipyridine derivative,is a second-generation COX-2-selective inhibitor with the highest selectivity ratio of any coxib for inhibition of COX-2 relative to COX-1.It is extensively metabolized by hepatic P450 enzymes followed by renal excretion and has an elimination half-life of 22 hours.Etoricoxib is approved in the United Kingdom for the treatment of the signs and symptoms of osteoarthritis(60 mg once daily)and rheumatoid arthritis(90 mg once daily),for treatment of acute gouty arthritis (120 mg once daily),and for relief of acute musculoskeletal pain(60 mg once daily).Approval in the USA is still pending.Ninety mg daily of etoricoxib has superior efficacy compared with 500 mg of naproxen twice daily in the treatment of rheumatoid arthritis over 12 weeks.Etoricoxib has similar efficacy to traditional NSAIDs for osteoarthritis,acute gouty arthritis,and primary dysmenorrhea and has a gastrointestinal safety profile similar to that of other coxibs.Since etoricoxib has structural similarities to diclofenac,it is appropriate to monitor hepatic function carefully in patients using this drug. 3.Meloxicam Meloxicam is an enolcarboxamide related to piroxicam that has been shown to preferentially inhibit COX-2 over COX-1,particularly at its lowest therapeutic dose of 7.5 mg/d.It is not as selective as the other coxibs and may be considered "preferentially"selective rather than "highly"selective.The drug is popular in Europe and many other countries for most rheumatic diseases and has recently been approved for treatment of osteoarthritis in the USA.Its efficacy in this condition and rheumatoid arthritis is comparable to that of other NSAIDs.It is associated with fewer clinical gastrointestinal symptoms and complications than piroxicam,diclofenac,and naproxen.Similarly,while meloxicam is known to inhibit synthesis of thromboxane A2,it appears that even at supratherapeutic doses its blockade of thromboxane A2 does not reach levels that result in decreased in vivo platelet function.Other toxicities are similar to those of other NSAIDs
Celecoxib is as effective as other NSAIDs in the treatment of rheumatoid arthritis and osteoarthritis, and in trials it has caused fewer endoscopic ulcers than most other NSAIDs. Probably because it is a sulfonamide, celecoxib may cause rashes. It does not affect platelet aggregation at usual doses. It interacts occasionally with warfarin¾as would be expected of a drug metabolized via CYP2C9. Although celecoxib is associated with about half the gastrointestinal side effects of nonselective NSAIDs, the frequency of other adverse effects approximates that of other NSAIDs. Celecoxib causes no more edema or renal effects than other members of the NSAID group, but edema and hypertension have been documented. 2. Etoricoxib Etoricoxib, a bipyridine derivative, is a second-generation COX-2-selective inhibitor with the highest selectivity ratio of any coxib for inhibition of COX-2 relative to COX-1. It is extensively metabolized by hepatic P450 enzymes followed by renal excretion and has an elimination half-life of 22 hours. Etoricoxib is approved in the United Kingdom for the treatment of the signs and symptoms of osteoarthritis (60 mg once daily) and rheumatoid arthritis (90 mg once daily), for treatment of acute gouty arthritis (120 mg once daily), and for relief of acute musculoskeletal pain (60 mg once daily). Approval in the USA is still pending. Ninety mg daily of etoricoxib has superior efficacy compared with 500 mg of naproxen twice daily in the treatment of rheumatoid arthritis over 12 weeks. Etoricoxib has similar efficacy to traditional NSAIDs for osteoarthritis, acute gouty arthritis, and primary dysmenorrhea and has a gastrointestinal safety profile similar to that of other coxibs. Since etoricoxib has structural similarities to diclofenac, it is appropriate to monitor hepatic function carefully in patients using this drug. 3. Meloxicam Meloxicam is an enolcarboxamide related to piroxicam that has been shown to preferentially inhibit COX-2 over COX-1, particularly at its lowest therapeutic dose of 7.5 mg/d. It is not as selective as the other coxibs and may be considered "preferentially" selective rather than "highly" selective. The drug is popular in Europe and many other countries for most rheumatic diseases and has recently been approved for treatment of osteoarthritis in the USA. Its efficacy in this condition and rheumatoid arthritis is comparable to that of other NSAIDs. It is associated with fewer clinical gastrointestinal symptoms and complications than piroxicam, diclofenac, and naproxen. Similarly, while meloxicam is known to inhibit synthesis of thromboxane A2, it appears that even at supratherapeutic doses its blockade of thromboxane A2 does not reach levels that result in decreased in vivo platelet function. Other toxicities are similar to those of other NSAIDs