26.In the treatment of malaria,primaquine is useful because of its ability to destroy malarial (1)primary tissue schizonts (2)blood schizonts (3)gametocytes (4)sporozoites 27.True statements regarding isoniazid include that it (1)is structurally similar to pyridoxine (2)inhibits the synthesis of mycolic acids (3)is metabolized by acetylation (4)can be hepatotoxic 28.Correct statements concerning cephalosporins in comparison with penicillins include which of the following? (1)Their structures are closely related (2)Their mechanism of action is analogous (3)Cephalosporins have an unusually broader antimicrobial spectrum (4)Their hypersensitivity reactions can produce similar symptoms including anaphylactic reactions 29.Penicillin has little or no antibacterial action against (1)Treponema pallidum (2)actively growing bacterial cells (3)meningococci (4)resting bacterial cells 30.Cardiotoxicity limits the clinical usefulness of which of the following antitumor antibiotics? (1)Dactinomycin (2)Doxorubicin (Adriamycin)(3)Bleomycin (4) Daunorubicin 31.Common complications of cephalothin therapy in hospitalized patients include
26. In the treatment of malaria, primaquine is useful because of its ability to destroy malarial (1) primary tissue schizonts (2) blood schizonts (3) gametocytes (4) sporozoites 27. True statements regarding isoniazid include that it (1) is structurally similar to pyridoxine (2) inhibits the synthesis of mycolic acids (3) is metabolized by acetylation (4) can be hepatotoxic 28. Correct statements concerning cephalosporins in comparison with penicillins include which of the following? (1) Their structures are closely related (2) Their mechanism of action is analogous (3) Cephalosporins have an unusually broader antimicrobial spectrum (4) Their hypersensitivity reactions can produce similar symptoms, including anaphylactic reactions 29. Penicillin has little or no antibacterial action against (1) Treponema pallidum (2) actively growing bacterial cells (3) meningococci (4) resting bacterial cells 30. Cardiotoxicity limits the clinical usefulness of which of the following antitumor antibiotics? (1) Dactinomycin (2) Doxorubicin (Adriamycin) (3) Bleomycin (4) Daunorubicin 31. Common complications of cephalothin therapy in hospitalized patients include
(1)fever,eosinophilia,and anaphylaxis (2)superinfection with G+ organisms (3)thrombophlebitis (4)hemolytic anemia 32.The acute toxic effects of methotrexate are reduced by the administration of (1)ascorbic acid (2)folic acid (3)niacin (4)tetrahydrofolate 33.Correct statements about the clinical application of carbenicillin include which of the following? (1)It frequently causes diarrhea (2)It is resistant to penicillinase (3)It can cause hyperkalemic alkalosis (4)It has greater activity against gram-negative bacteria than penicillin G 34.Resistance to penicillinase is found in which of the following penicillins? (1)Ampicillin (2)Oxacillin (3)Carbenicillin (4)Dicloxacillin 35.Second-generation cephalosporins include (1)cefazolin (2)cefuroxime (3)cefotaxime (4)cefamandole 36.Metronidazole is an effective treatment for which of the following infectious diseases? (1)Amebiasis (2)Air way inflammatory disease (3)Trichomonas infections (4)Moniliasis 37.Probenecid is sometimes given as an adjuvant in penicillin therapy because probenecid (1)inhibits the renal tubular transport of penicillin (2)has a synergistic bactericidal action with penicillin (3)allows for higher serum levels of penicillin
(1) fever, eosinophilia, and anaphylaxis (2) superinfection with G+ organisms (3) thrombophlebitis (4) hemolytic anemia 32. The acute toxic effects of methotrexate are reduced by the administration of (1) ascorbic acid (2) folic acid (3) niacin (4) tetrahydrofolate 33. Correct statements about the clinical application of carbenicillin include which of the following? (1)It frequently causes diarrhea (2)It is resistant to penicillinase (3)It can cause hyperkalemic alkalosis (4)It has greater activity against gram-negative bacteria than penicillin G 34. Resistance to penicillinase is found in which of the following penicillins? (1)Ampicillin (2)Oxacillin (3)Carbenicillin (4)Dicloxacillin 35.Second-generation cephalosporins include (1)cefazolin (2)cefuroxime (3)cefotaxime (4)cefamandole 36. Metronidazole is an effective treatment for which of the following infectious diseases? (1) Amebiasis (2) Air way inflammatory disease (3) Trichomonas infections (4) Moniliasis 37. Probenecid is sometimes given as an adjuvant in penicillin therapy because probenecid (1) inhibits the renal tubular transport of penicillin (2) has a synergistic bactericidal action with penicillin (3) allows for higher serum levels of penicillin
(4)enhances directly the diffusion of penicillin through bacterial membranes 38.Causal prophylaxis of malarial infections may be achieved by treatment with (1)quinine (2)primaquine (3)chloroquine (4)pyrimethamine 39.Sulfonamides may cause renal damage that has been shown to be the result of precipitation of crystals in the collecting tubules of the kidney.Predisposing factors to such crystal formation include (1)high urinary concentration of the drug (2)low urinary solubility of the drug (3)a urine pH of less than 5.0 (4)simultaneous administration of several sulfonamides 41.An infection caused by extraintestinal entamoeba histolytica can be effectively treated with (1)metronidazole (2)tinidazole (3)chloroquine (4)iodoquinol 42.Aminoglycosides frequently are combined with another antibiotic to treat certain infections.The reasons for employing such combinations include (1)obtaining a synergistic effect (2)preventing the emergence of resistant bacteria(3)increasing the antimicrobial spectrum (4) increasing oral absorption 43.Resistance of bacteria to penicillins can be caused by which of the following? (1)B-Lactamase (2)amidase activity (3)modified PBPs (4) Decarboxylase activity 44.The activity of dihydrofolate reductase is inhibited by (1)SD (2)trimethoprim (3)sulfisoxazole (4)pyrimethamine 45.Neuro (1)Neomycin (2)Polymyxin (3)Streptomycin (4)Penicillin
(4) enhances directly the diffusion of penicillin through bacterial membranes 38. Causal prophylaxis of malarial infections may be achieved by treatment with (1)quinine (2) primaquine (3) chloroquine (4) pyrimethamine 39. Sulfonamides may cause renal damage that has been shown to be the result of precipitation of crystals in the collecting tubules of the kidney. Predisposing factors to such crystal formation include (1) high urinary concentration of the drug (2) low urinary solubility of the drug (3) a urine pH of less than 5.0 (4) simultaneous administration of several sulfonamides 41. An infection caused by extraintestinal Entamoeba histolytica can be effectively treated with (1) metronidazole (2) tinidazole (3) chloroquine (4) iodoquinol 42. Aminoglycosides frequently are combined with another antibiotic to treat certain infections. The reasons for employing such combinations include (1) obtaining a synergistic effect (2) preventing the emergence of resistant bacteria(3) increasing the antimicrobial spectrum (4) increasing oral absorption 43. Resistance of bacteria to penicillins can be caused by which of the following? (1) ß-Lactamase (2) amidase activity (3) modified PBPs (4) Decarboxylase activity 44. The activity of dihydrofolate reductase is inhibited by (1)SD (2)trimethoprim (3)sulfisoxazole (4)pyrimethamine 45. Neuromuscular blockade produced by tubocurarine is potentiated by which of the following agents? (1) Neomycin (2) Polymyxin (3) Streptomycin (4) Penicillin
46.Bacterial protein synthesis is directly inhibited by which of the following antibiotics? (1)Rifampin (2)Chloramphenicol (3)Penicillin (4)Tetracycline 47.Truestatements cephalosprin of the following? (1)Cephalosporins are bactericidal against multiplying bacteria (2)Cephalosporins and penicillins have a similar spectrum of activity (3)Cross-hypersensitivity exists between cephalosporins and penicillins (4)Cephalosporins are resistant to inactivation by B-lactamases 48.Correct statements concerning the adverse reactions caused by aminoglycosides include (1)produce ototoxicity (2)are common and potent neuromuscular blockers (3)produce nephrotoxicity during or after use (4)have a high incidence of hypersensitivity reactions similar to those of penicillins 49.The pharmacologic properties of amphotericin B include (1)effectiveness when administered orally (2)usefulness in the treatment of systemic mycoses (3)damage of membrane (4)severe renal toxicity 50.Drugs considered to be cell-cycle specific include (1)5-fluorouracil (2)methotrexate (3)6-mercaptopurine (4) vincristine 51.Inhibition of the sulfonamide bacteriostatic mechanism can occur by the administration of (1)acetylsalicylate (2)folic acid (3)vitamin B6 (4) p-aminobenzoic acid
46. Bacterial protein synthesis is directly inhibited by which of the following antibiotics? (1) Rifampin (2) Chloramphenicol (3) Penicillin (4) Tetracycline 47. True statements concerning cephalosporin antibiotics include which of the following? (1) Cephalosporins are bactericidal against multiplying bacteria (2) Cephalosporins and penicillins have a similar spectrum of activity (3) Cross-hypersensitivity exists between cephalosporins and penicillins (4) Cephalosporins are resistant to inactivation by ß-1actamases 48. Correct statements concerning the adverse reactions caused by aminoglycosides include (1) produce ototoxicity (2) are common and potent neuromuscular blockers (3) produce nephrotoxicity during or after use (4) have a high incidence of hypersensitivity reactions similar to those of penicillins 49. The pharmacologic properties of amphotericin B include (1) effectiveness when administered orally (2) usefulness in the treatment of systemic mycoses (3) damage of membrane (4) severe renal toxicity 50. Drugs considered to be cell-cycle specific include (1) 5-fluorouracil (2) methotrexate (3) 6-mercaptopurine (4) vincristine 51. Inhibition of the sulfonamide bacteriostatic mechanism can occur by the administration of (1) acetylsalicylate (2) folic acid (3) vitamin B6 (4) p-aminobenzoic acid
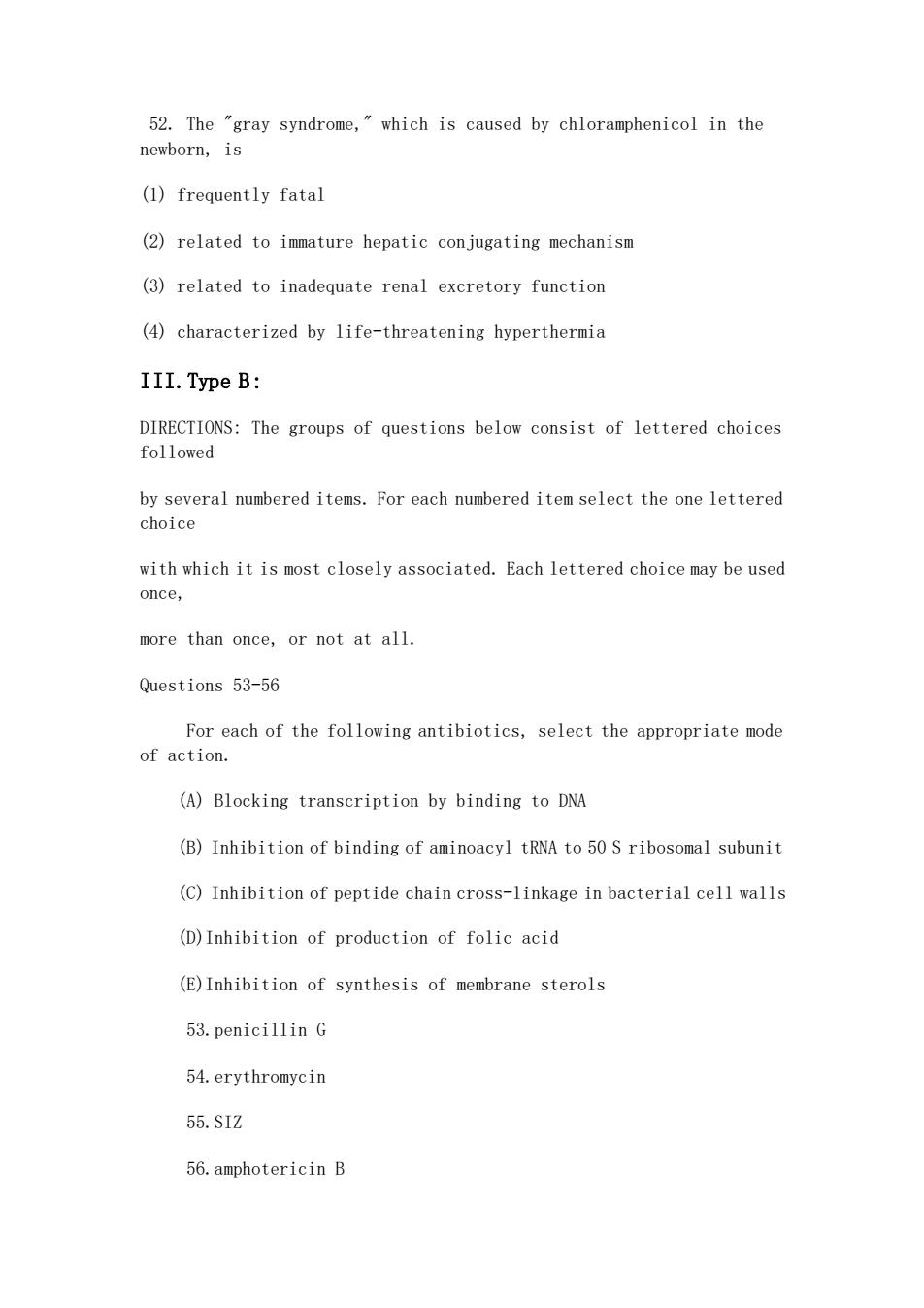
52.The "gray syndrome,which is caused by chloramphenicol in the newborn,is (1)frequently fatal (2)related to immature hepatic conjugating mechanism (3)related to inadequate renal excretory function (4)characterized by life-threatening hyperthermia III.Type B: DIRECTIONS:The groups of questions below consist of lettered choices followed by several numbered items.For each numbered item select the one lettered choice with which it is most closely associated.Each lettered choice may be used once, more than once,or not at all Questions 53-56 For each of the following antibiotics,select the appropriate mode of action. (A)Blocking transcription by binding to DNA (B)Inhibition of binding of aminoacyl tRNA to 50 S ribosomal subunit (C)Inhibition of peptide chain cross-linkage in bacterial cell walls (D)Inhibition of production of folic acid (E)Inhibition of synthesis of membrane sterols 53.penicillin G 54.erythromycin 55.SIZ 56.amphotericin B
52. The "gray syndrome," which is caused by chloramphenicol in the newborn, is (1) frequently fatal (2) related to immature hepatic conjugating mechanism (3) related to inadequate renal excretory function (4) characterized by life-threatening hyperthermia III.Type B: DIRECTIONS: The groups of questions below consist of lettered choices followed by several numbered items. For each numbered item select the one lettered choice with which it is most closely associated. Each lettered choice may be used once, more than once, or not at all. Questions 53-56 For each of the following antibiotics, select the appropriate mode of action. (A) Blocking transcription by binding to DNA (B) Inhibition of binding of aminoacyl tRNA to 50 S ribosomal subunit (C) Inhibition of peptide chain cross-linkage in bacterial cell walls (D)Inhibition of production of folic acid (E)Inhibition of synthesis of membrane sterols 53.penicillin G 54.erythromycin 55.SIZ 56.amphotericin B