Integrated Management of Pregnancy and Childbirth Pregnancy,Childbirth,Postpartum and Newborn Care: A guide for essential practice 2nd Edition ●●● World Health Organization ●●UNFPA unicef ●●● The World Bank Group Department of Making Pregnancy Safer
Department of Making Pregnancy Safer 2nd Edition

FOREWORD In modern times,improvements in knowledge and technological advances have greatly improved the It is against this background that we are proud to present the document Pregnancy,Childbirth. health of mother and children.However,the past decade was marked by limited progress in reducing Postpartum and Newbor Care:A guide for essential practice,as new additions to the Integrated matemal mortality and a slow-down in the steady decline of childhood mortality observed since the Management of Pregnancy and Childbirth tool kit.The guide provides a full range of updated, mid 1950s in many countries,the latter being largely due to a failure to reduce neonatal mortality. evidence-based norms and standards that will enable health care providers to give high quality care during pregnancy.delivery and in the postpartum period,considering the needs of the mother and her Every year,over four million babies less than one month of age die,most of them during the critical newborn baby. first week of life:and for every newborn who dies,another is stillborn.Most of these deaths are a consequence of the poor health and nutritional status of the mother coupled with inadequate care We hope that the guide will be helpful for decision-makers,programme managers and health care before,during.and after delivery.Unfortunately,the problem remains unrecognized or-worse-accepted providers in charting out their roadmap towards meeting the health needs of all mothers and children. as inevitable in many societies,in large part because it is so common. We have the knowledge,our major challenge now is to translate this into action and to reach those women and children who are most in need. Recognizing the large burden of matemnal and neonatal ill-health on the development capacity of individuals.communities and societies,world leaders reaffirmed their commitment to invest in mothers and children by adopting specific goals and targets to reduce matemal and childhood-infant mortality as part of the Millennium Declaration. There is a widely shared but mistaken idea that improvements in newbom health require sophisticated and expensive technologies and highly specialized staff.The reality is that many conditions that result in perinatal death can be prevented or treated without sophisticated and expensive technology.What is required is essential care during pregnancy,the assistance of a person with midwifery skills during Dr.Tomris Turmen childbirth and the immediate postpartum period,and a few critical interventions for the newbom Executive director during the first days of life. Family and Community Health(FCH) QHOM3HO Foreword
Foreword FOREWORD In modern times, improvements in knowledge and technological advances have greatly improved the health of mother and children. However, the past decade was marked by limited progress in reducing maternal mortality and a slow-down in the steady decline of childhood mortality observed since the mid 1950s in many countries, the latter being largely due to a failure to reduce neonatal mortality. Every year, over four million babies less than one month of age die, most of them during the critical first week of life; and for every newborn who dies, another is stillborn. Most of these deaths are a consequence of the poor health and nutritional status of the mother coupled with inadequate care before, during, and after delivery. Unfortunately, the problem remains unrecognized or- worse- accepted as inevitable in many societies, in large part because it is so common. Recognizing the large burden of maternal and neonatal ill-health on the development capacity of individuals, communities and societies, world leaders reaffirmed their commitment to invest in mothers and children by adopting specific goals and targets to reduce maternal and childhood-infant mortality as part of the Millennium Declaration. There is a widely shared but mistaken idea that improvements in newborn health require sophisticated and expensive technologies and highly specialized staff. The reality is that many conditions that result in perinatal death can be prevented or treated without sophisticated and expensive technology. What is required is essential care during pregnancy, the assistance of a person with midwifery skills during childbirth and the immediate postpartum period, and a few critical interventions for the newborn during the first days of life. It is against this background that we are proud to present the document Pregnancy, Childbirth, Postpartum and Newborn Care: A guide for essential practice, as new additions to the Integrated Management of Pregnancy and Childbirth tool kit. The guide provides a full range of updated, evidence-based norms and standards that will enable health care providers to give high quality care during pregnancy, delivery and in the postpartum period, considering the needs of the mother and her newborn baby. We hope that the guide will be helpful for decision-makers, programme managers and health care providers in charting out their roadmap towards meeting the health needs of all mothers and children. We have the knowledge, our major challenge now is to translate this into action and to reach those women and children who are most in need. Dr. Tomris Türmen Executive director Family and Community Health (FCH) FOREWORD
Acknowledgements SIN3 ACKNOWLEDGEMENTS 远 The Guide was prepared by a team of the World Health Organization.Department of Reproductive This guide represents a common understanding between WHO.UNFPA,UNICEF and the World Bank Health and Research(RHR).led by Jerker Liljestrand and Jelka Zupan. of key elements of an approach to reducing matemal and perinatal mortality and morbidity.These agencies co-operate closely in efforts to reduce maternal and perinatal mortality and morbidity. The concept and first drafts were developed by Sandra Gove and Patricia Whitesell/ACT Intemational, The principles and policies of each agency are govemed by the relevant decisions of each agency's Atlanta,Jerker Liljestrand.Denise Roth.Betty Sweet.Anne Thompson,and Jelka Zupan. goveming body and each agency implements the interventions described in this document in accordance with these principles and policies and within the scope of its mandate. Revisions were subsequently carried out by Annie Portela,Luc de Bemis.Omella Lincetto,Rita Kabra. Maggie Usher,Agostino Borra,Rick Guidotti,Elisabeth Hoff,Mathews Matthai,Monir Islam, The guide has also been reviewed and endorsed by the International Confederation of Midwives,the Felicity Savage,Adepeyu Olukoya,Aafje Rietveld,TinTin Sint,Ekpini Ehounu,Suman Mehta. International Federation of Gynecology and Obstetrics and Intemational Pediatric Association. Valuable inputs were provided by WHO Regional Offices and WHO departments: Reproductive Health and Research Child and Adolescent Health and Development ■HV/AIDS Communicable Diseases Nutrition for Health and Development Intemational Essential Drugs and Medicines Policy Gm6 calgy and正srks PedlatricAssodation Vaccines and Biologicals Mental Health and Substance Dependence The financial support towards the preparation and production of this document provided by UNFPA and Gender and Women's Health the Governments of Australia.Japan and the United States of America is gratefully acknowledged. Blindness and Deafness as is financial support received from The World Bank.In addition,WHO's Making Pregnancy Safer initiative is grateful to the programme support received from the Govemments of the Netherlands. Editing:Nina Mattock,Richard Casna Norway,Sweden and the United Kingdom of Great Britain and Northem Ireland. Layout:rsdesigns.com sarl Cover design:Maire Ni Mhearain WHO acknowledges with gratitude the generous contribution of over 100 individuals and organizations in the field of matemal and newborn health,who took time to review this document at different stages of its development They came from over 35 countries and brought their expertise and wide experence to the final text
ACKNOWLEDGEMENTS The Guide was prepared by a team of the World Health Organization, Department of Reproductive Health and Research (RHR), led by Jerker Liljestrand and Jelka Zupan. The concept and first drafts were developed by Sandra Gove and Patricia Whitesell/ACT International, Atlanta, Jerker Liljestrand, Denise Roth, Betty Sweet, Anne Thompson, and Jelka Zupan. Revisions were subsequently carried out by Annie Portela, Luc de Bernis, Ornella Lincetto, Rita Kabra, Maggie Usher, Agostino Borra, Rick Guidotti, Elisabeth Hoff, Mathews Matthai, Monir Islam, Felicity Savage, Adepeyu Olukoya, Aafje Rietveld, TinTin Sint, Ekpini Ehounu, Suman Mehta. Valuable inputs were provided by WHO Regional Offices and WHO departments: N Reproductive Health and Research N Child and Adolescent Health and Development N HIV/AIDS N Communicable Diseases N Nutrition for Health and Development N Essential Drugs and Medicines Policy N Vaccines and Biologicals N Mental Health and Substance Dependence N Gender and Women’s Health N Blindness and Deafness Editing: Nina Mattock, Richard Casna Layout: rsdesigns.com sàrl Cover design: Maíre Ní Mhearáin WHO acknowledges with gratitude the generous contribution of over 100 individuals and organizations in the field of maternal and newborn health, who took time to review this document at different stages of its development. They came from over 35 countries and brought their expertise and wide experience to the final text. This guide represents a common understanding between WHO, UNFPA, UNICEF, and the World Bank of key elements of an approach to reducing maternal and perinatal mortality and morbidity. These agencies co-operate closely in efforts to reduce maternal and perinatal mortality and morbidity. The principles and policies of each agency are governed by the relevant decisions of each agency’s governing body and each agency implements the interventions described in this document in accordance with these principles and policies and within the scope of its mandate. The guide has also been reviewed and endorsed by the International Confederation of Midwives, the International Federation of Gynecology and Obstetrics and International Pediatric Association. The financial support towards the preparation and production of this document provided by UNFPA and the Governments of Australia, Japan and the United States of America is gratefully acknowledged, as is financial support received from The World Bank. In addition, WHO’s Making Pregnancy Safer initiative is grateful to the programme support received from the Governments of the Netherlands, Norway, Sweden and the United Kingdom of Great Britain and Northern Ireland. Acknowledgements ACKNOWLEDGEMENTS International Pediatric Association International Confederation of Midwives International Federation of Gynecology and Obstetrics
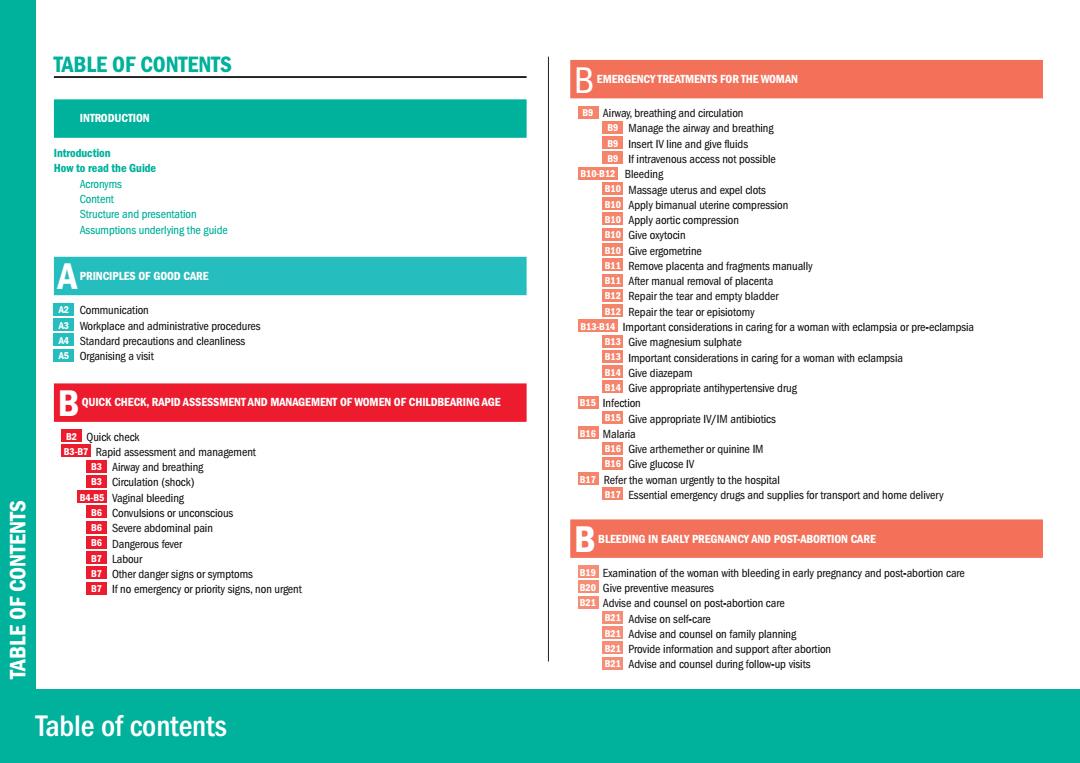
TABLE OF CONTENTS B EMERGENCY TREATMENTS FOR THE WOMAN INTRODUCTION B Airway,breathing and circulation Manage the airway and breathing B Insert IV line and give fluids Introduction If intravenous access not possible How to read the Guide E1002 Bleeding Acronyms Massage uterus and expel clots Content Apply bimanual uterine compression Structure and presentation B10 Apply aortic compression Assumptions underlying the guide B10 Give oxytocin B10 Give ergometrine Remove placenta and fragments manually PRINCIPLES OF GOOD CARE After manual removal of placenta Repair the tear and empty bladder A2: Communication Repair the tear or episiotomy A好 Workplace and administrative procedures Important considerations in caring for a woman with eclampsia or pre-eclampsia M Standard precautions and cleanliness Eh Give magnesium sulphate 5Organising a visit Important considerations in caring for a woman with eclampsia B Give diazepam Give appropriate antihypertensive drug QUICK CHECK.RAPID ASSESSMENT AND MANAGEMENT OF WOMEN OF CHILDBEARING AGE 15Infection Give appropriate IV/IM antibiotics 2 Quick check B16 Malaria B6-B Rapid assessment and management GGive arthemether or quinine IM Bs Airway and breathing ENG Give glucose IV B3 Circulation(shock) Refer the woman urgently to the hospital B4-85 Vaginal bleeding Essential emergency drugs and supplies for transport and home delivery B6 Corulsions or unconscious SIN3INOO 86 Severe abdominal pain B6 Dangerous fever BLEEDING IN EARLY PREGNANCY AND POST-ABORTION CARE B7 Labour Other danger signs or symptoms Examination of the woman with bleeding in early pregnancy and post-abortion care If no emergency or priority signs,non urgent 20 Give preventive measures Advise and counsel on post-abortion care Advise on self-care Advise and counsel on family planning B21 Provide information and support after abortion Advise and counsel during follow-up visits Table of contents
Table of contents TABLE OF CONTENTS TABLE OF CONTENTS A INTRODUCTION Introduction How to read the Guide Acronyms Content Structure and presentation Assumptions underlying the guide A PRINCIPLES OF GOOD CARE A2 Communication A3 Workplace and administrative procedures A4 Standard precautions and cleanliness A5 Organising a visit B QUICK CHECK, RAPID ASSESSMENT AND MANAGEMENT OF WOMEN OF CHILDBEARING AGE B2 Quick check B3-B7 Rapid assessment and management B3 Airway and breathing B3 Circulation (shock) B4-B5 Vaginal bleeding B6 Convulsions or unconscious B6 Severe abdominal pain B6 Dangerous fever B7 Labour B7 Other danger signs or symptoms B7 If no emergency or priority signs, non urgent BEMERGENCY TREATMENTS FOR THE WOMAN B9 Airway, breathing and circulation B9 Manage the airway and breathing B9 Insert IV line and give fluids B9 If intravenous access not possible B10-B12 Bleeding B10 Massage uterus and expel clots B10 Apply bimanual uterine compression B10 Apply aortic compression B10 Give oxytocin B10 Give ergometrine B11 Remove placenta and fragments manually B11 After manual removal of placenta B12 Repair the tear and empty bladder B12 Repair the tear or episiotomy B13-B14 Important considerations in caring for a woman with eclampsia or pre-eclampsia B13 Give magnesium sulphate B13 Important considerations in caring for a woman with eclampsia B14 Give diazepam B14 Give appropriate antihypertensive drug B15 Infection B15 Give appropriate IV/IM antibiotics B16 Malaria B16 Give arthemether or quinine IM B16 Give glucose IV B17 Refer the woman urgently to the hospital B17 Essential emergency drugs and supplies for transport and home delivery B BLEEDING IN EARLY PREGNANCY AND POST-ABORTION CARE B19 Examination of the woman with bleeding in early pregnancy and post-abortion care B20 Give preventive measures B21 Advise and counsel on post-abortion care B21 Advise on self-care B21 Advise and counsel on family planning B21 Provide information and support after abortion B21 Advise and counsel during follow-up visits

Table of contents SIN3INOO ANTENATAL CARE D CHILDBIRTH-LABOUR,DELIVERY AND IMMEDIATE POSTPARTUM CARE Assess the pregnant woman:pregnancy status,birth and emergency plan D2 Examine the woman in labour or with ruptured membranes Check for pre-eclampsia Decide stage of labour C4 Check for anaemia DD5 Respond to obstetrical problems on admission 5Check for syphilis DGive supportive care throughout labour C Check for HIV status DCommunication Respond to observed signs or volunteered problems D6 Cleanliness If no fetal movement D6 Mobility C7 If ruptured membranes and no labour D6 Urination C8 If fever or burning on urination D3 Eating.drinking c9 If vaginal discharge D6 Breathing technique If signs suggesting HIV infection Pain and discomfort relief c10 If smoking.alcohol or drug abuse,or history of violence D Birth companion G11 If cough or breathing difficulty D3 First stage of labour If taking antituberculosis drugs DB Not in active labour Give preventive measures D9 In active labour Advise and counsel on nutrition and self-care Second stage of labour:deliver the baby and give immediate newbom care Develop a birth and emergency plan Third stage of labour:deliver the placenta Facility delivery Respond to problems during labour and delivery c14 Home delivery with a skilled attendant DIf fetal heart rate <120 or>160 beats per minute G15 Advise on labour signs D15 If prolapsed cord C5Advise on danger signs D1G If breech presentation Discuss how to prepare for an emergency in pregnancy If stuck shoulders(Shoulder dystocia) GAdvise and counsel on family planning D3 If multiple births 16 Counsel on the importance of family planning Care of the mother and newborn within first hour of delivery of placenta Special consideration for family planning counselling during pregnancy Care of the mother one hour after delivery of placenta Advise on routine and follow-up visits Assess the mother after delivery C18 Home delivery without a skilled attendant Respond to problems immediately postpartum Assess eligibility of ARV for HIV-positive pregnant woman If vaginal bleeding 22If fever (temperature >38C) If perineal tear or episiotomy(done for lifesaving circumstances) If elevated diastolic blood pressure 0 If pallor on screening.check for anaemia 20If mother severely ill or separated from the child 0 If baby stillbom or dead D25 Give preventive measures
Table of contents TABLE OF CONTENTS C ANTENATAL CARE C2 Assess the pregnant woman: pregnancy status, birth and emergency plan C3 Check for pre-eclampsia C4 Check for anaemia C5 Check for syphilis C6 Check for HIV status C7 Respond to observed signs or volunteered problems C7 If no fetal movement C7 If ruptured membranes and no labour C8 If fever or burning on urination C9 If vaginal discharge C10 If signs suggesting HIV infection C10 If smoking, alcohol or drug abuse, or history of violence C11 If cough or breathing difficulty C11 If taking antituberculosis drugs C12 Give preventive measures C13 Advise and counsel on nutrition and self-care C14-C15 Develop a birth and emergency plan C14 Facility delivery C14 Home delivery with a skilled attendant C15 Advise on labour signs C15 Advise on danger signs C15 Discuss how to prepare for an emergency in pregnancy C16 Advise and counsel on family planning C16 Counsel on the importance of family planning C16 Special consideration for family planning counselling during pregnancy C17 Advise on routine and follow-up visits C18 Home delivery without a skilled attendant C19 Assess eligibility of ARV for HIV-positive pregnant woman D CHILDBIRTH – LABOUR, DELIVERY AND IMMEDIATE POSTPARTUM CARE D2 Examine the woman in labour or with ruptured membranes D3 Decide stage of labour D4-D5 Respond to obstetrical problems on admission D6-D7 Give supportive care throughout labour D6 Communication D6 Cleanliness D6 Mobility D6 Urination D6 Eating, drinking D6 Breathing technique D6 Pain and discomfort relief D7 Birth companion D8-D9 First stage of labour D8 Not in active labour D9 In active labour D10-D11 Second stage of labour: deliver the baby and give immediate newborn care D12-D13 Third stage of labour: deliver the placenta D14-D18 Respond to problems during labour and delivery D14 If fetal heart rate <120 or >160 beats per minute D15 If prolapsed cord D16 If breech presentation D17 If stuck shoulders (Shoulder dystocia) D18 If multiple births D19 Care of the mother and newborn within first hour of delivery of placenta D20 Care of the mother one hour after delivery of placenta D21 Assess the mother after delivery D22-D25 Respond to problems immediately postpartum D22 If vaginal bleeding D22 If fever (temperature >38°C) D22 If perineal tear or episiotomy (done for lifesaving circumstances) D23 If elevated diastolic blood pressure D24 If pallor on screening, check for anaemia D24 If mother severely ill or separated from the child D24 If baby stillborn or dead D25 Give preventive measures