CHILDBIRTH-LABOUR.DELIVERY AND IMMEDIATE POSTPARTUM CARE (CONTINUED PREVENTIVE MEASURES AND ADDITIONAL TREATMENTS FOR THE WOMAN 2G Advise on postpartum care 2Preventive measures 2G Advise on postpartum care and hygiene Give tetanus toxoid D25 Counsel on nutrition Give vitamin A postpartum Counsel on birth spacing and family planning Give iron and folic acid Counsel on the importance of family planning Give mebendazole D2 Lactation amenorrhea method (LAM) Motivate on compliance with iron treatment 23 Advise on when to return ROGive preventive intermittent treatment for falciparum malaria 23 Routine postpartum visits Advise to use insecticide-treated bednet 2Follow-up visits for problems Give appropriate oral antimalarial treatment 2 Advise on danger signs R Give paracetamol 2Discuss how to prepare for an emergency in postpartum Additional treatments for the woman Home delivery by skilled attendant Give appropriate oral antibiotics 2Preparation for home delivery Give benzathine penicillin IM D2 Delivery care 3 Observe for signs of allergy 2Immediate postpartum care of mother 2Postpartum care of newborn POSTPARTUM CARE Postpartum examination of the mother(up to 6 weeks) 3 Respond to observed signs or volunteered problems If elevated diastolic blood pressure 3 If pallor.check for anaemia Check for HIV status E6 If heavy vaginal bleeding E5 If fever or foul-smelling lochia If dribbling urine If pus or perineal pain If feeling unhappy or crying easily 3If vaginal discharge 4 weeks after delivery 告 33 If breast problem EIf cough or breathing difficulty If taking anti-tuberculosis drugs If signs suggesting HIV infection Table of contents
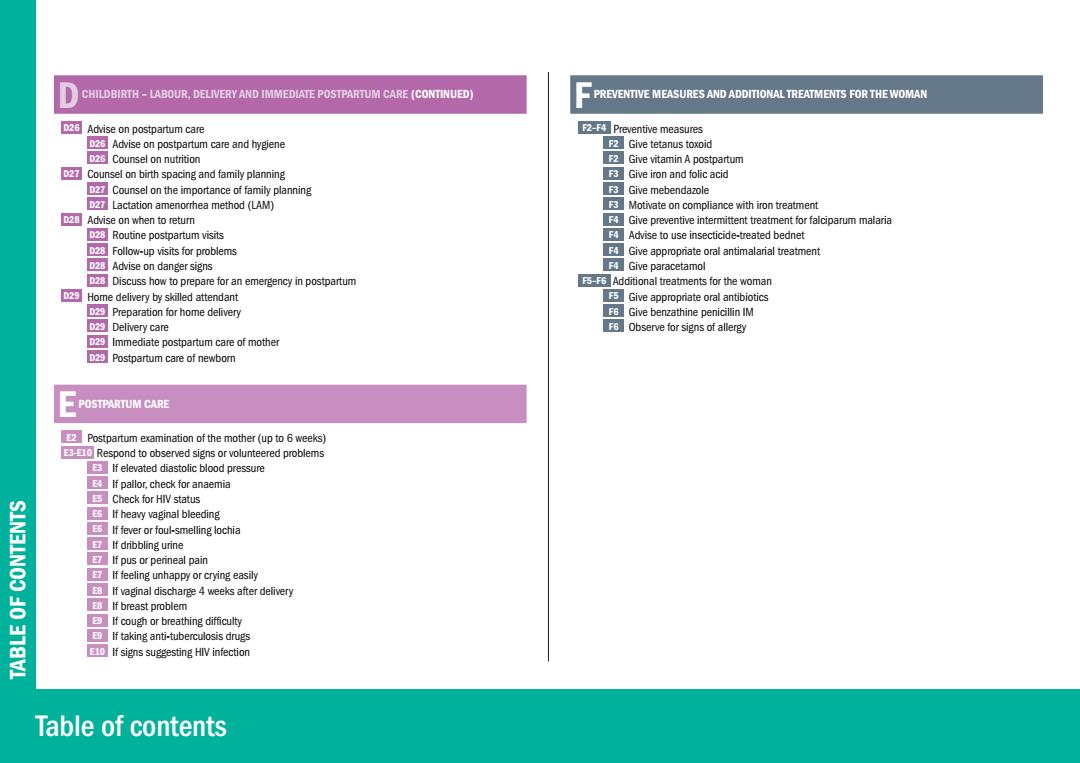
Table of contents TABLE OF CONTENTS D CHILDBIRTH – LABOUR, DELIVERY AND IMMEDIATE POSTPARTUM CARE (CONTINUED) D26 Advise on postpartum care D26 Advise on postpartum care and hygiene D26 Counsel on nutrition D27 Counsel on birth spacing and family planning D27 Counsel on the importance of family planning D27 Lactation amenorrhea method (LAM) D28 Advise on when to return D28 Routine postpartum visits D28 Follow-up visits for problems D28 Advise on danger signs D28 Discuss how to prepare for an emergency in postpartum D29 Home delivery by skilled attendant D29 Preparation for home delivery D29 Delivery care D29 Immediate postpartum care of mother D29 Postpartum care of newborn E POSTPARTUM CARE E2 Postpartum examination of the mother (up to 6 weeks) E3-E10 Respond to observed signs or volunteered problems E3 If elevated diastolic blood pressure E4 If pallor, check for anaemia E5 Check for HIV status E6 If heavy vaginal bleeding E6 If fever or foul-smelling lochia E7 If dribbling urine E7 If pus or perineal pain E7 If feeling unhappy or crying easily E8 If vaginal discharge 4 weeks after delivery E8 If breast problem E9 If cough or breathing difficulty E9 If taking anti-tuberculosis drugs E10 If signs suggesting HIV infection F PREVENTIVE MEASURES AND ADDITIONAL TREATMENTS FOR THE WOMAN F2–F4 Preventive measures F2 Give tetanus toxoid F2 Give vitamin A postpartum F3 Give iron and folic acid F3 Give mebendazole F3 Motivate on compliance with iron treatment F4 Give preventive intermittent treatment for falciparum malaria F4 Advise to use insecticide-treated bednet F4 Give appropriate oral antimalarial treatment F4 Give paracetamol F5–F6 Additional treatments for the woman F5 Give appropriate oral antibiotics F6 Give benzathine penicillin IM F6 Observe for signs of allergy
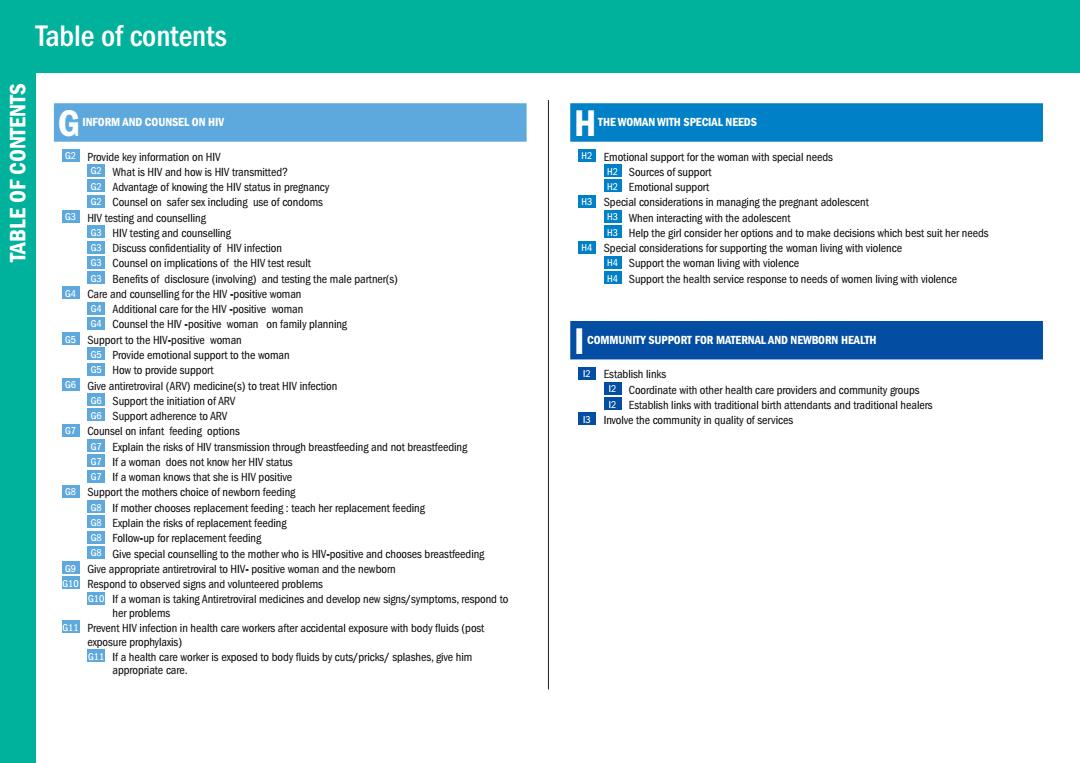
Table of contents SIN3INOO G NFORM AND COUNSEL ON HIV H THE WOMAN WITH SPECIAL NEEDS Provide key information on HIV 2 Emotional support for the woman with special needs What is HIV and how is HIV transmitted? 2 Sources of support GAdvantage of knowing the HIV status in pregnancy 2Emotional support Counsel on safer sex including use of condoms Special considerations in managing the pregnant adolescent GHIV testing and counselling GEWhen interacting with the adolescent G3 HIV testing and counselling Help the girl consider her options and to make decisions which best suit her needs 63 Discuss confidentiality of HIV infection Special considerations for supporting the woman living with violence G3 Counsel on implications of the HIV test result HSupport the woman living with violence Benefits of disclosure (involving)and testing the male partner(s) Support the health service response to needs of women living with violence Care and counselling for the HIV-positive woman Additional care for the HIV-positive woman G4 Counsel the HIV-positive woman on family planning 5Support to the HIV-positive woman COMMUNITY SUPPORT FOR MATERNAL AND NEWBORN HEALTH Provide emotional support to the woman C5How to provide support 2Establish links 06 Give antiretroviral (ARV)medicine(s)to treat HIV infection 2 Coordinate with other health care providers and community groups Support the initiation of ARV Establish links with traditional birth attendants and traditional healers Support adherence to ARV Involve the community in quality of services Counsel on infant feeding options Explain the risks of HIV transmission through breastfeeding and not breastfeeding o If a woman does not know her HIV status If a woman knows that she is HIV positive Support the mothers choice of newbom feeding G If mother chooses replacement feeding:teach her replacement feeding GB Explain the risks of replacement feeding G8 Follow-up for replacement feeding Give special counselling to the mother who is HlV-positive and chooses breastfeeding Give appropriate antiretroviral to HIV-positive woman and the newbor 10 Respond to observed signs and volunteered problems If a woman is taking Antiretroviral medicines and develop new signs/symptoms,respond to her problems 旺国 Prevent HIV infection in health care workers after accidental exposure with body fluids(post exposure prophylaxis) If a health care worker is exposed to body fluids by cuts/pricks/splashes,give him appropriate care
Table of contents TABLE OF CONTENTS G INFORM AND COUNSEL ON HIV G2 Provide key information on HIV G2 What is HIV and how is HIV transmitted? G2 Advantage of knowing the HIV status in pregnancy G2 Counsel on safer sex including use of condoms G3 HIV testing and counselling G3 HIV testing and counselling G3 Discuss confidentiality of HIV infection G3 Counsel on implications of the HIV test result G3 Benefits of disclosure (involving) and testing the male partner(s) G4 Care and counselling for the HIV -positive woman G4 Additional care for the HIV -positive woman G4 Counsel the HIV -positive woman on family planning G5 Support to the HIV-positive woman G5 Provide emotional support to the woman G5 How to provide support G6 Give antiretroviral (ARV) medicine(s) to treat HIV infection G6 Support the initiation of ARV G6 Support adherence to ARV G7 Counsel on infant feeding options G7 Explain the risks of HIV transmission through breastfeeding and not breastfeeding G7 If a woman does not know her HIV status G7 If a woman knows that she is HIV positive G8 Support the mothers choice of newborn feeding G8 If mother chooses replacement feeding : teach her replacement feeding G8 Explain the risks of replacement feeding G8 Follow-up for replacement feeding G8 Give special counselling to the mother who is HIV-positive and chooses breastfeeding G9 Give appropriate antiretroviral to HIV- positive woman and the newborn G10 Respond to observed signs and volunteered problems G10 If a woman is taking Antiretroviral medicines and develop new signs/symptoms, respond to her problems G11 Prevent HIV infection in health care workers after accidental exposure with body fluids (post exposure prophylaxis) G11 If a health care worker is exposed to body fluids by cuts/pricks/ splashes, give him appropriate care. H THE WOMAN WITH SPECIAL NEEDS H2 Emotional support for the woman with special needs H2 Sources of support H2 Emotional support H3 Special considerations in managing the pregnant adolescent H3 When interacting with the adolescent H3 Help the girl consider her options and to make decisions which best suit her needs H4 Special considerations for supporting the woman living with violence H4 Support the woman living with violence H4 Support the health service response to needs of women living with violence I COMMUNITY SUPPORT FOR MATERNAL AND NEWBORN HEALTH I2 Establish links I2 Coordinate with other health care providers and community groups I2 Establish links with traditional birth attendants and traditional healers I3 Involve the community in quality of services
四 Other breastfeeding support NEWBORN CARE 超 Give special support to the mother who is not yet breastfeeding If the baby does not have a mother 2 Examine the newbom Advise the mother who is not breastfeeding at all on how to relieve engorgement If preterm,birth weight <2500 g or twin a Ensure warmth for the baby Assess breastfeeding @ Keep the baby warm Check for special treatment needs Keep a small baby warm J6 Look for signs of jaundice and local infection @ Rewarm the baby skin-to-skin 7 If danger signs Other baby care 8 If swelling,bruises or malformation Cord care Assess the mother's breasts if complaining of nipple or breast pain Sleeping 10 Care of the newborn 0Hygiene 11 Additional care of a small baby (or twin) Newborn resuscitation 2 Assess replacement feeding 型 Keep the baby warm Open the airway 1 If still not breathing,ventilate BREASTFEEDING,CARE,PREVENTIVE MEASURES AND TREATMENT FOR THE NEWBORN If breathing less than 30 breaths per minute or severe chest in-drawing.stop ventilating If not breathing or gasping at all after 20 minutes of ventilation Counsel on breastfeeding Treat and immunize the baby 应 Counsel on importance of exclusive breastfeeding Treat the baby 12 Give 2 IM antibiotics (first week of life) Help the mother to initiate breastfeeding 3 Support exclusive breastfeeding K12 Give IM benzathine penicillin to baby (single dose)if mother tested RPR-positive 3 Teach comect positioning and attachment for breastfeeding Give IM antibiotic for possible gonococcal eye infection(single dose) Give special support to breastfeed the small baby (preterm and/or low birth weight) Teach the mother to give treatment to the baby at home M K13 Give special support to breastfeed twins Treat local infection GAlternative feeding methods 13 Give isoniazid (INH)prophylaxis to newbom 13 Express breast milk Immunize the newborn Hand express breast milk directly into the baby's mouth Give antiretroviral (ARV)medicine to newborn Cup feeding expressed breast milk Advise when to retum with the baby 船 14 Quantity to feed by cup Routine visits Signs that baby is receiving adequate amount of milk Follow-up visits Weigh and assess weight gain 14 Advise the mother to seek care for the baby Weigh baby in the first month of life 14 Refer baby urgently to hospital Assess weight gain 告 Scale maintenance Table of contents
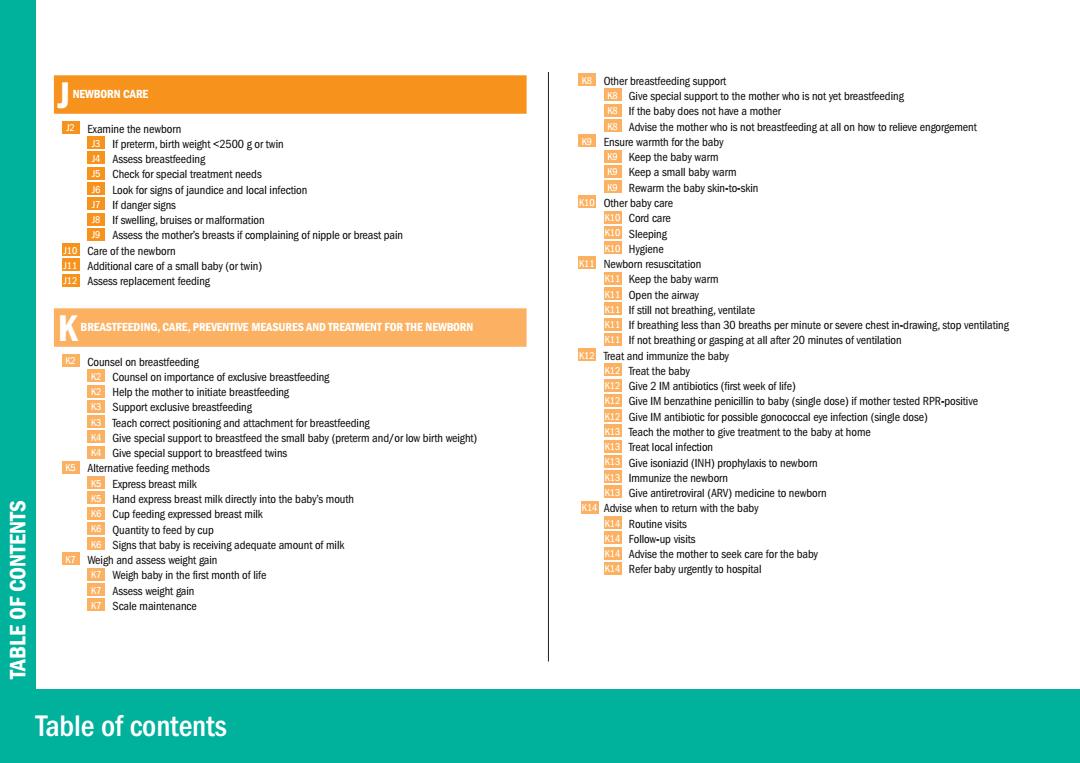
Table of contents TABLE OF CONTENTS J NEWBORN CARE J2 Examine the newborn J3 If preterm, birth weight <2500 g or twin J4 Assess breastfeeding J5 Check for special treatment needs J6 Look for signs of jaundice and local infection J7 If danger signs J8 If swelling, bruises or malformation J9 Assess the mother’s breasts if complaining of nipple or breast pain J10 Care of the newborn J11 Additional care of a small baby (or twin) J12 Assess replacement feeding K BREASTFEEDING, CARE, PREVENTIVE MEASURES AND TREATMENT FOR THE NEWBORN K2 Counsel on breastfeeding K2 Counsel on importance of exclusive breastfeeding K2 Help the mother to initiate breastfeeding K3 Support exclusive breastfeeding K3 Teach correct positioning and attachment for breastfeeding K4 Give special support to breastfeed the small baby (preterm and/or low birth weight) K4 Give special support to breastfeed twins K5 Alternative feeding methods K5 Express breast milk K5 Hand express breast milk directly into the baby’s mouth K6 Cup feeding expressed breast milk K6 Quantity to feed by cup K6 Signs that baby is receiving adequate amount of milk K7 Weigh and assess weight gain K7 Weigh baby in the first month of life K7 Assess weight gain K7 Scale maintenance K8 Other breastfeeding support K8 Give special support to the mother who is not yet breastfeeding K8 If the baby does not have a mother K8 Advise the mother who is not breastfeeding at all on how to relieve engorgement K9 Ensure warmth for the baby K9 Keep the baby warm K9 Keep a small baby warm K9 Rewarm the baby skin-to-skin K10 Other baby care K10 Cord care K10 Sleeping K10 Hygiene K11 Newborn resuscitation K11 Keep the baby warm K11 Open the airway K11 If still not breathing, ventilate K11 If breathing less than 30 breaths per minute or severe chest in-drawing, stop ventilating K11 If not breathing or gasping at all after 20 minutes of ventilation K12 Treat and immunize the baby K12 Treat the baby K12 Give 2 IM antibiotics (first week of life) K12 Give IM benzathine penicillin to baby (single dose) if mother tested RPR-positive K12 Give IM antibiotic for possible gonococcal eye infection (single dose) K13 Teach the mother to give treatment to the baby at home K13 Treat local infection K13 Give isoniazid (INH) prophylaxis to newborn K13 Immunize the newborn K13 Give antiretroviral (ARV) medicine to newborn K14 Advise when to return with the baby K14 Routine visits K14 Follow-up visits K14 Advise the mother to seek care for the baby K14 Refer baby urgently to hospital
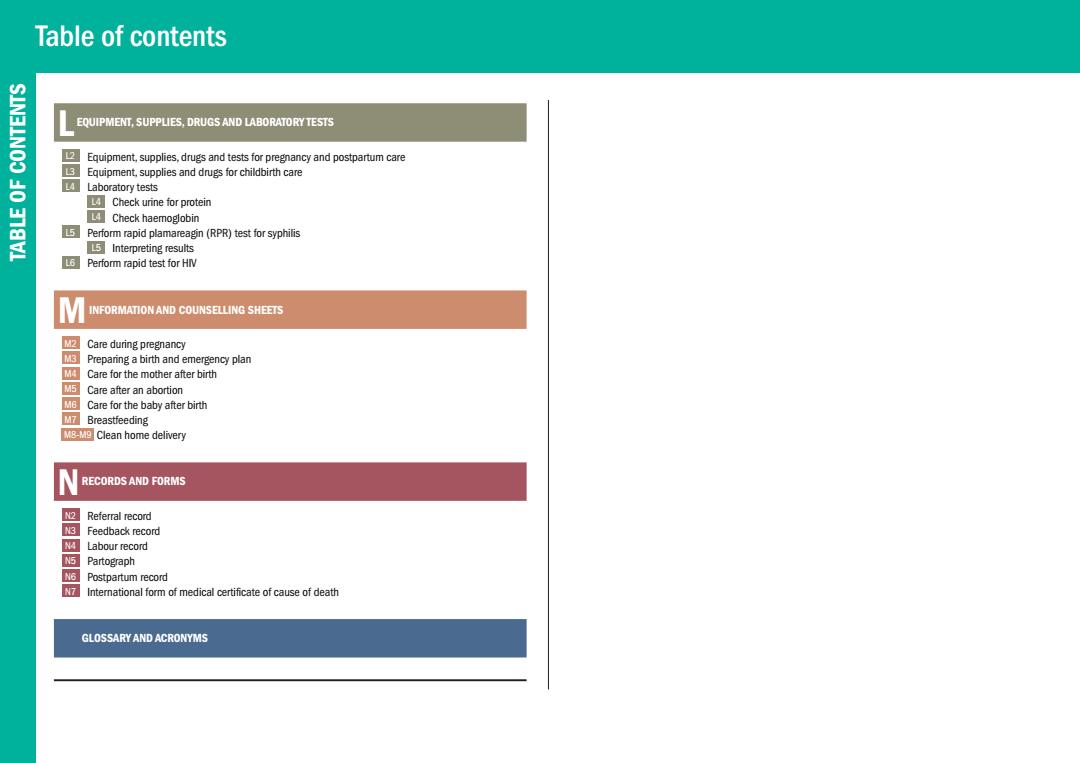
Table of contents SIN3LNOO EQUIPMENT,SUPPLIES,DRUGS AND LABORATORY TESTS 2 Equipment,supplies,drugs and tests for pregnancy and postpartum care 3 Equipment,supplies and drugs for childbirth care 告 LA Laboratory tests Check urine for protein 18V Check haemoglobin Perform rapid plamareagin(RPR)test for syphilis 5Interpreting results 6 Perform rapid test for HIV INFORMATION AND COUNSELLING SHEETS M2 Care during pregnancy Preparing a birth and emergency plan Care for the mother after birth M5 Care after an abortion Care for the baby after birth MZ Breastfeeding E Clean home delivery RECORDS AND FORMS 2 Referral record Feedback record Labour record 阿 Partograph Postpartum record International form of medical certificate of cause of death GLOSSARY AND ACRONYMS
Table of contents TABLE OF CONTENTS L EQUIPMENT, SUPPLIES, DRUGS AND LABORATORY TESTS L2 Equipment, supplies, drugs and tests for pregnancy and postpartum care L3 Equipment, supplies and drugs for childbirth care L4 Laboratory tests L4 Check urine for protein L4 Check haemoglobin L5 Perform rapid plamareagin (RPR) test for syphilis L5 Interpreting results L6 Perform rapid test for HIV M INFORMATION AND COUNSELLING SHEETS M2 Care during pregnancy M3 Preparing a birth and emergency plan M4 Care for the mother after birth M5 Care after an abortion M6 Care for the baby after birth M7 Breastfeeding M8-M9 Clean home delivery N RECORDS AND FORMS N2 Referral record N3 Feedback record N4 Labour record N5 Partograph N6 Postpartum record N7 International form of medical certificate of cause of death O GLOSSARY AND ACRONYMS
INTRODUCTION The aim of Pregnancy,childbirth,postpartum and newborn care guide for essential practice (PCPNC)is The Guide has been developed by the Department of Reproductive Health and Research with to provide evidence-based recommendations to guide health care professionals in the management of contributions from the following WHO programmes: women during pregnancy,childbirth and postpartum,and post abortion,and newboms during their first week of life,including management of endemic diseases like malaria,HIV/AIDS,TB and anaemia. Child and Adolesscent Health and Development ■HV/AIDS All recommendations are for skilled attendants working at the primary level of health care,either at the Nutrition for Health and Development facility or in the community.They apply to all women attending antenatal care,in delivery,postpartum Essential drugs and Medicines Policy or post abortion care,or who come for emergency care,and to all newbomns at birth and during the first Vaccines and Biologicals week of life (or later)for routine and emergency care. Communicable Diseases Control.Prevention and Eradication(tuberculosis.malaria.helminthiasis) Gender and Women's Health The PCPNC is a guide for clinical decision-making.It facilitates the collection,analysis,classification and Mental Health and Substance Dependence use of relevant information by suggesting key questions,essential observations and/or examinations, Blindness and Deafness and recommending appropriate research-based interventions.It promotes the early detection of complications and the initiation of early and appropriate treatment,including timely referral,if necessary. Correct use of this guide should help reduce the high maternal and perinatal mortality and morbidity rates prevalent in many parts of the developing world,thereby making pregnancy and childbirth safer. The guide is not designed for immediate use.It is a generic guide and should first be adapted to local needs and resources.It should cover the most serious endemic conditions that the skilled birth attendant must be able to treat,and be made consistent with national treatment guidelines and other policies.It is accompanied by an adaptation guide to help countries prepare their own national guides and training and other supporting materials NOILO The first section,How to use the guide,describes how the guide is organized,the overall content and presentation.Each chapter begins with a short description of how to read and use it,to help the reader use the guide correctly. Introduction
The aim of Pregnancy, childbirth, postpartum and newborn care guide for essential practice (PCPNC) is to provide evidence-based recommendations to guide health care professionals in the management of women during pregnancy, childbirth and postpartum, and post abortion, and newborns during their first week of life, including management of endemic diseases like malaria, HIV/AIDS, TB and anaemia. All recommendations are for skilled attendants working at the primary level of health care, either at the facility or in the community. They apply to all women attending antenatal care, in delivery, postpartum or post abortion care, or who come for emergency care, and to all newborns at birth and during the first week of life (or later) for routine and emergency care. The PCPNC is a guide for clinical decision-making. It facilitates the collection, analysis, classification and use of relevant information by suggesting key questions, essential observations and/or examinations, and recommending appropriate research-based interventions. It promotes the early detection of complications and the initiation of early and appropriate treatment, including timely referral, if necessary. Correct use of this guide should help reduce the high maternal and perinatal mortality and morbidity rates prevalent in many parts of the developing world, thereby making pregnancy and childbirth safer. The guide is not designed for immediate use. It is a generic guide and should first be adapted to local needs and resources. It should cover the most serious endemic conditions that the skilled birth attendant must be able to treat, and be made consistent with national treatment guidelines and other policies. It is accompanied by an adaptation guide to help countries prepare their own national guides and training and other supporting materials. The first section, How to use the guide, describes how the guide is organized, the overall content and presentation. Each chapter begins with a short description of how to read and use it, to help the reader use the guide correctly. The Guide has been developed by the Department of Reproductive Health and Research with contributions from the following WHO programmes: N Child and Adolesscent Health and Development N HIV/AIDS N Nutrition for Health and Development N Essential drugs and Medicines Policy N Vaccines and Biologicals N Communicable Diseases Control, Prevention and Eradication (tuberculosis, malaria, helminthiasis) N Gender and Women’s Health N Mental Health and Substance Dependence N Blindness and Deafness INTRODUCTION INTRODUCTION Introduction