
FACTORS WHICH PROMOTE BLOOD FLUIDITY Normal Hemostasis Natural Anticoagulants Protein C Protein S Antithrombin III Endothelial-Derived Anti-Platelet Substances Nitric Oxide Prostacyclin(PGl2) Fibrinolytic System "clot busters" Plasmin Plasminogen Tissue Plasminogen Activator(tPA) Department of Pharmacology Howard University College of Medicine

上游充通大淫 SHANGHAI JIAO TONG UNIVERSITY 1896 1920 1987 2006 History of Anticoagulants Jay McLean,a second year medical student at Johns Hopkins University,discovered this wonderful drug in 1916 while performing research in the laboratory of W.H.Howell,MD. W&LI 1三 In 1960,DW Barritt and SC Jordan performed the first randomized trial showing the efficacy of anticoagulant therapy in the treatment of venous thromboembolism. Since then,important therapeutic advances have been made in the treatment of deep venous thrombosis and pulmonary embolism. .Barritt,D.W.,and Jordan,S.C.:Anticoagulant drugs in the treatment of pulmonary embolism.A controlled trial.Lancet,1:1309-1312,1960.[Medlinel
History of Anticoagulants In 1960, DW Barritt and SC Jordan performed the first randomized trial showing the efficacy of anticoagulant therapy in the treatment of venous thromboembolism. Since then, important therapeutic advances have been made in the treatment of deep venous thrombosis and pulmonary embolism. •Barritt, D. W., and Jordan, S. C.: Anticoagulant drugs in the treatment of pulmonary embolism. A controlled trial. Lancet, 1: 1309-1312, 1960.[Medline] Jay McLean, a second year medical student at Johns Hopkins University, discovered this wonderful drug in 1916 while performing research in the laboratory of W.H. Howell, MD
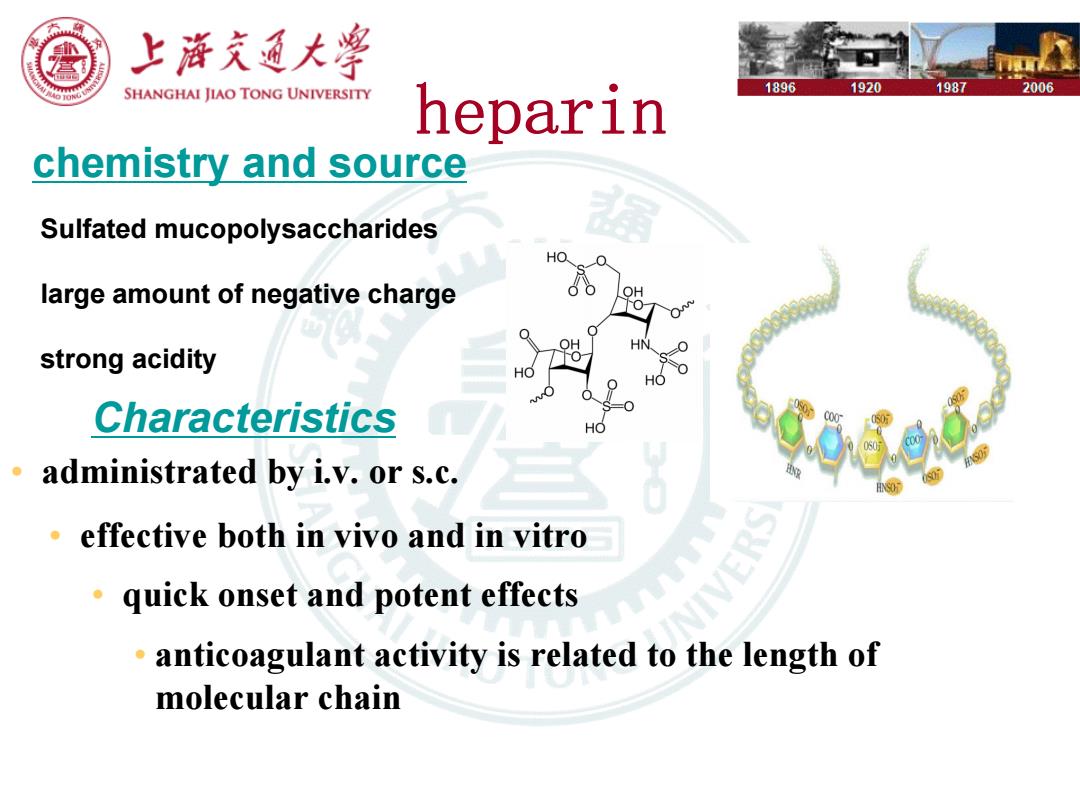
上游充通大学 SHANGHAI JIAO TONG UNIVERSITY 1896 1920 1987 2006 heparin chemistry and source Sulfated mucopolysaccharides large amount of negative charge strong acidity Characteristics administrated by i.v.or s.c. effective both in vivo and in vitro quick onset and potent effects anticoagulant activity is related to the length of molecular chain
heparin chemistry and source Sulfated mucopolysaccharides large amount of negative charge strong acidity Characteristics • administrated by i.v. or s.c. • effective both in vivo and in vitro • quick onset and potent effects • anticoagulant activity is related to the length of molecular chain

上降充通大警 SHANGHAI IIAO TONG UNIVERSITY 1896 1920 1987 2006 heparin---Mechanism Heparin works by inhibiting the three major clotting factors (thrombin,thromboplastin,and prothrombin). It slows the process of thromboplastin synthesis,decelerates the conversion of prothrombin to thrombin,and inhibits the effects of thrombin on fibrinogen,blocking its conversion to fibrin. heparin heparin AT Ill thrombin' AT III thrombin* heparin heparin AT IlI thrombin AT Ill thrombin* can also be Factor Xa
heparin AT III thrombin* AT III heparin thrombin* thrombin* heparin AT III AT III thrombin* heparin Fig. 50-3 * can also be Factor Xa heparin---Mechanism Heparin works by inhibiting the three major clotting factors (thrombin, thromboplastin, and prothrombin). It slows the process of thromboplastin synthesis, decelerates the conversion of prothrombin to thrombin, and inhibits the effects of thrombin on fibrinogen, blocking its conversion to fibrin
上浒充通大 SHANGHAI JIAO TONG UNIVERSITY 1896 1920 1987 2006 Heparin Heparin is given by injection or drip into a vein (intravenously)or by injection under the skin (subcutaneously)for treatment and prevention. It is derived from porcine intestinal mucosa, standardized for anticoagulant activity. The agent also causes an increase in the 客图1 Heparin number of negatively charged ions in the Sodium Injection,S 1000 USP units/1 mL vascular wall,which helps prevent the 前mL Multiple Dose V SU6 CUTANE005峡 formation of intravascular clots
Heparin • Heparin is given by injection or drip into a vein (intravenously) or by injection under the skin (subcutaneously) for treatment and prevention. • It is derived from porcine intestinal mucosa, standardized for anticoagulant activity. • The agent also causes an increase in the number of negatively charged ions in the vascular wall, which helps prevent the formation of intravascular clots