Factors affecting drug treatment of hypertension: Accuracy of diagnosis;severity of hypertension Etiology:Primary(essential hypertension)vs.secondary (10-15%patients) Identifiable causes of hypertension:Pheochromocytoma,renal artery constriction,Cushing's syndrome(hypercorticism)and Cushing's disease (over-production of ACTH),primary aldosteronism,thyroid or parathyroid disease,coarctation of the aorta Pre-existing risk factors and medical conditions(smoking,hyperlipidemia, diabetes,congestive heart failure,asthma,current medications) Individualization(age,gender,ethnicity);patient compliance Single drug(monotherapy)vs.multiple drug(polypharmacy)
Factors affecting drug treatment of hypertension: • Accuracy of diagnosis; severity of hypertension • Etiology: Primary (essential hypertension) vs. secondary (10-15% patients) • Identifiable causes of hypertension: Pheochromocytoma, renal artery constriction, Cushing’s syndrome (hypercorticism) and Cushing’s disease (over-production of ACTH), primary aldosteronism, thyroid or parathyroid disease, coarctation of the aorta • Pre-existing risk factors and medical conditions (smoking, hyperlipidemia, diabetes, congestive heart failure, asthma, current medications) • Individualization (age, gender, ethnicity); patient compliance • Single drug (monotherapy) vs. multiple drug (polypharmacy)
Development of AHDs-Chronology 1930 Veratrum alkaloids(affect sensitivity of baroreceptors;not currently in use due to toxicity) 1940 Thiocyanates(sodium nitroprusside);ganglion blocking agents (trimethaphan) 1950 Catecholamine depletors(reserpine);vasodilators(hydralazine);PNS sympathetic inhibitors(guanethidine);MAO inhibitors(pargyline);diuretics (hydrochlorothiazides) 1960 CNS a2 agonists(clonidine);beta blockers(propranolol);methyldopa 1970 Alpha1 blockers(prazocin);alpha/beta blockers(labetalol);ACE inhibitors (captopril) 1980 Calcium channel blockers(nimodipine) 1990 Angiotensin-ll receptor antagonists(losartan) 2000 Endothelin receptor antagonists(bosentan)
Development of AHDs - Chronology 1930 Veratrum alkaloids (affect sensitivity of baroreceptors; not currently in use due to toxicity) 1940 Thiocyanates (sodium nitroprusside); ganglion blocking agents (trimethaphan) 1950 Catecholamine depletors (reserpine); vasodilators (hydralazine); PNS sympathetic inhibitors (guanethidine); MAO inhibitors (pargyline); diuretics (hydrochlorothiazides) 1960 CNS agonists (clonidine); beta blockers (propranolol); methyldopa 1970 Alpha1 blockers (prazocin); alpha/beta blockers (labetalol); ACE inhibitors (captopril) 1980 Calcium channel blockers (nimodipine) 1990 Angiotensin-II receptor antagonists (losartan) 2000 Endothelin receptor antagonists (bosentan)
Pharmacological mechanism-based classification ACE inhibitors and AT-lI receptor antagonists: ACE inhbitors-captopril,enalapril,enalaprilat,lisinopril,benazepril AT-lI receptor antagonists-losartan Calcium channel blockers:nifedipine,amlodipine,felodipine,diltiazem,verapamil Diuretics: Thiazide-Hydrochlorothiazide Loop-furosemide,torsemide,ethacrynic acid Potassium-sparing-amiloride,spironolactone,triamterene Sympathoplegic agents: Adrenergic synthesis release blockers-reserpine,granethidine Central a-adrenergic agonists-a-methodopa,clonidine a-blockers-prazosin,tetrazosin,doxazosin B-blockers-propranolol,nadolol,timolol,metoprolol,acebutolol,penbutolol,pindolol Ganglion blocker-Trimethaphan Direct vasodilators:hydralazine,minoxidil,sodium nitroprusside,diazoxide
Pharmacological mechanism-based classification ACE inhibitors and AT-II receptor antagonists: ACE inhbitors – captopril, enalapril, enalaprilat, lisinopril, benazepril AT-II receptor antagonists - losartan Calcium channel blockers: nifedipine, amlodipine, felodipine, diltiazem, verapamil Diuretics: Thiazide - Hydrochlorothiazide Loop - furosemide, torsemide, ethacrynic acid Potassium-sparing - amiloride, spironolactone, triamterene Sympathoplegic agents: Adrenergic synthesis / release blockers - reserpine, granethidine Central -adrenergic agonists – -methodopa, clonidine blockers - prazosin, tetrazosin, doxazosin blockers - propranolol, nadolol, timolol, metoprolol, acebutolol, penbutolol, pindolol Ganglion blocker - Trimethaphan Direct vasodilators: hydralazine, minoxidil, sodium nitroprusside, diazoxide
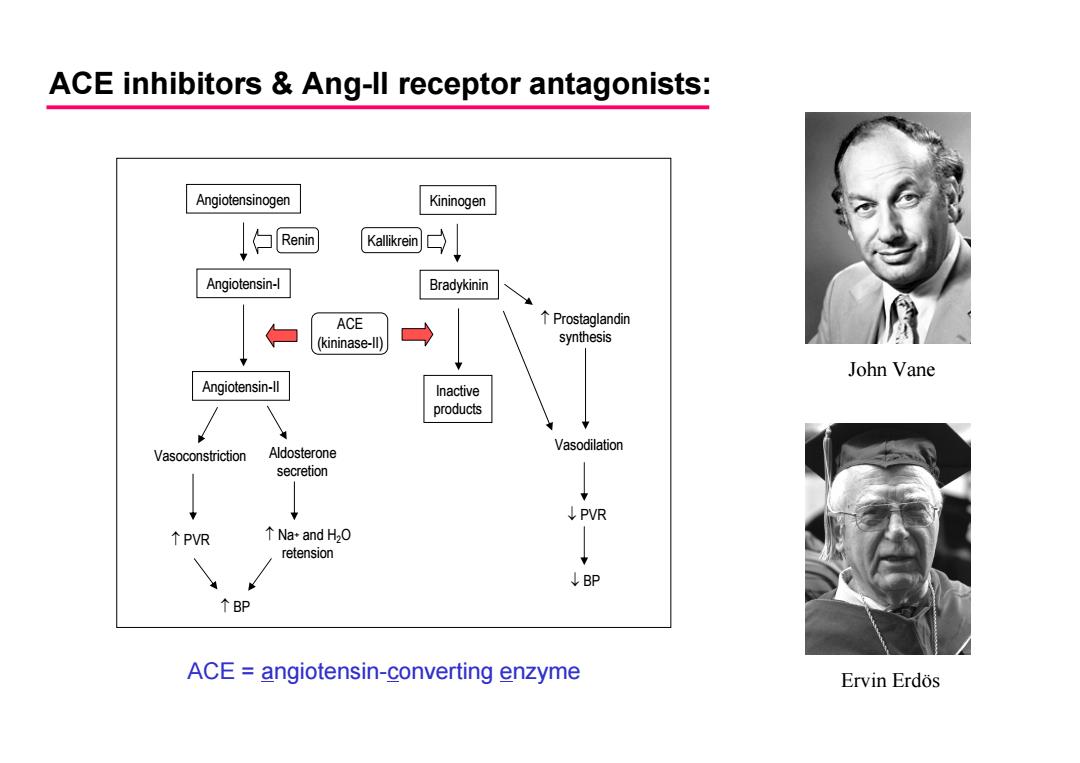
ACE inhibitors Ang-ll receptor antagonists: Angiotensinogen Kininogen Renin Kallikrein Angiotensin-l Bradykinin ACE 个Prostaglandin (kininase-ll) synthesis John Vane Angiotensin-lI Inactive products Vasoconstriction Aldosterone Vasodilation secretion ↓PVR ↑PVR ↑Na+and H2(0 retension ↓BP ↑BP ACE angiotensin-converting enzyme Ervin Erdos
Angiotensinogen Angiotensin-I Angiotensin-II Vasoconstriction Aldosterone secretion PVR Na+ and H2O retension BP Bradykinin Kininogen Renin Kallikrein ACE (kininase-II) Inactive products Prostaglandin synthesis Vasodilation PVR BP ACE inhibitors & Ang-II receptor antagonists: ACE = angiotensin-converting enzyme John Vane Ervin Erdös
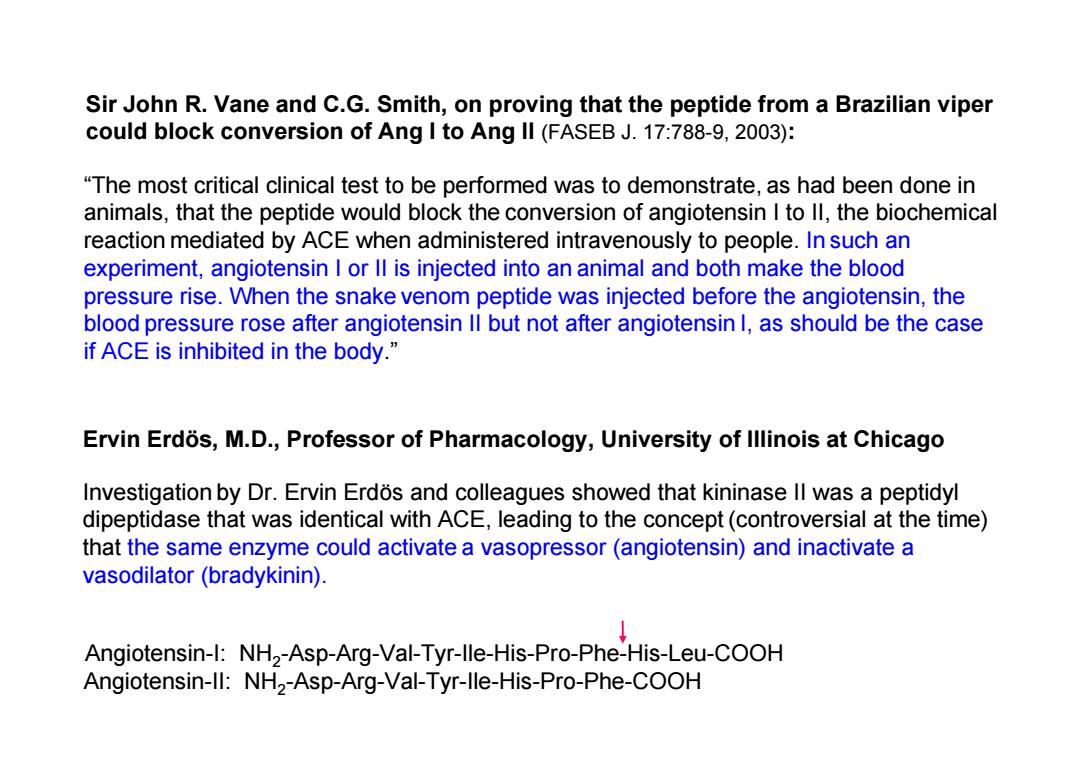
Sir John R.Vane and C.G.Smith,on proving that the peptide from a Brazilian viper could block conversion of Ang I to Ang ll(FASEB J.17:788-9,2003): "The most critical clinical test to be performed was to demonstrate,as had been done in animals,that the peptide would block the conversion of angiotensin I to ll,the biochemical reaction mediated by ACE when administered intravenously to people.In such an experiment,angiotensin I or ll is injected into an animal and both make the blood pressure rise.When the snake venom peptide was injected before the angiotensin,the blood pressure rose after angiotensin ll but not after angiotensin 1,as should be the case if ACE is inhibited in the body.' Ervin Erdos,M.D.,Professor of Pharmacology,University of Illinois at Chicago Investigation by Dr.Ervin Erdos and colleagues showed that kininase ll was a peptidyl dipeptidase that was identical with ACE,leading to the concept(controversial at the time) that the same enzyme could activate a vasopressor(angiotensin)and inactivate a vasodilator(bradykinin). Angiotensin-I:NH2-Asp-Arg-Val-Tyr-lle-His-Pro-Phe-His-Leu-COOH Angiotensin-ll:NH2-Asp-Arg-Val-Tyr-lle-His-Pro-Phe-COOH
“The most critical clinical test to be performed was to demonstrate, as had been done in animals, that the peptide would block the conversion of angiotensin I to II, the biochemical reaction mediated by ACE when administered intravenously to people. In such an experiment, angiotensin I or II is injected into an animal and both make the blood pressure rise. When the snake venom peptide was injected before the angiotensin, the blood pressure rose after angiotensin II but not after angiotensin I, as should be the case if ACE is inhibited in the body.” Sir John R. Vane and C.G. Smith, on proving that the peptide from a Brazilian viper could block conversion of Ang I to Ang II (FASEB J. 17:788-9, 2003): Investigation by Dr. Ervin Erdös and colleagues showed that kininase II was a peptidyl dipeptidase that was identical with ACE, leading to the concept (controversial at the time) that the same enzyme could activate a vasopressor (angiotensin) and inactivate a vasodilator (bradykinin). Ervin Erdös, M.D., Professor of Pharmacology, University of Illinois at Chicago Angiotensin-I: NH 2-Asp-Arg-Val-Tyr-Ile-His-Pro-Phe-His-Leu-COOH Angiotensin-II: NH 2-Asp-Arg-Val-Tyr-Ile-His-Pro-Phe-COOH