Exercise 1 oil-immersion objective,and use the fine adjustment to bring specimen into proper focus. e.To remove specimen,turn course adjustment knob in the direction tha makes the objective travel away from the slide.Remove microscope slide eaeswhestscheacpostaaec 10X 40X 60X Oil Immersion 100X SECOND SESSION FOCI:Gram Stain Technique,Characterization of Isolated Colonies A.Colony Morphology of Isolated Colonies and Pure Cultures >> 1.Check the TSA medium plates that were inoculated via the streak plate method for the presence of separate distinct colonies.Describe the cultural characteristics of these isolated colonies as to their size and shape. 2.Pure cultures of individual microorganisms are obtained by picking up a separated colony with a sterile inoculating needle or loop and streaking another plate of medium with this material.After 24 hours of incubation one should have an entire plate of one specific microorganism,and such pure cultures are then used to perform various tests and inoculations so that the bacterium can be identified according to its enzymaticaction on various substrates. 3.Prior to determining the metabolic activity of unknown bacteria, microorganisms are first identified based upon their morphology,namely their staining reaction,size,shape,pigment production,motility,and presence of capsules or spores.Gram stain several of the isolated colonies from the M-H streak plate and attempt to identify them morphologically 4.Pure cultures of Staphylococcus epidermidis and Pseudomonas geruginosa on M-H media will be available for student examination. Describe the cultural colony characteristics of these microorganisms and look for pigment production.Gram stain these bacteria and identify their microscopic morphology. Staphylococcus epidermidis Pseudomonas aeruginosa B.Differential gram stain >>> Prepare a smear of Escherichia coli on one end of the slide and a smear of file:///Desktop/clown/Microb Lab Web 2001/Exercise1/exercise1b.htm(5 of6)[8/3/00 :9:54 PM]
oil-immersion objective, and use the fine adjustment to bring specimen into proper focus. e. To remove specimen, turn course adjustment knob in the direction that makes the objective travel away from the slide. Remove microscope slide and always clean lens with lens tissue before proceeding to examine the next specimen. 10X 40X 60X Oil Immersion 100X SECOND SESSION FOCI: Gram Stain Technique, Characterization of Isolated Colonies A. Colony Morphology of Isolated Colonies and Pure Cultures >>>>> 1. Check the TSA medium plates that were inoculated via the streak plate method for the presence of separate distinct colonies. Describe the cultural characteristics of these isolated colonies as to their size and shape. 2. Pure cultures of individual microorganisms are obtained by picking up a separated colony with a sterile inoculating needle or loop and streaking another plate of medium with this material. After 24 hours of incubation, one should have an entire plate of one specific microorganism, and such pure cultures are then used to perform various tests and inoculations so that the bacterium can be identified according to its enzymatic action on various substrates. 3. Prior to determining the metabolic activity of unknown bacteria, microorganisms are first identified based upon their morphology, namely their staining reaction, size, shape, pigment production, motility, and presence of capsules or spores. Gram stain several of the isolated colonies from the M-H streak plate and attempt to identify them morphologically. 4. Pure cultures of Staphylococcus epidermidis and Pseudomonas aeruginosa on M-H media will be available for student examination. Describe the cultural colony characteristics of these microorganisms and look for pigment production. Gram stain these bacteria and identify their microscopic morphology. Staphylococcus epidermidis Pseudomonas aeruginosa B. Differential gram stain >>>>> Prepare a smear of Escherichia coli on one end of the slide and a smear of Exercise 1 file:///C|/WINDOWS/Desktop/clown/Microb Lab Web 2001/Exercise1/exercise1b.htm (5 of 6) [8/31/2002 4:29:54 PM]

Exercise1 Staphylococcus epidermidis on the other end of the slide.Preparing a smear from an agar culture(surface bacterial growth on solid medium)is a little more difficult and takes practice to obtain a good concentration(see SESSION 1:B.2). Gram stain and examine under the microscope as in session one IMAGES: 10X mag 40X mag 60X mag Oil immersion Gram stain of mixed culture S.epidermidis on M-H P.aureginosa on M-H file:///C/WINDOWS/Desktop/clown/Microb Lab Web 2001/Exercise1/exercise1b.htm(6 of 6)[8/31/2002 4:29:54 PM]
Staphylococcus epidermidis on the other end of the slide. Preparing a smear from an agar culture (surface bacterial growth on solid medium) is a little more difficult and takes practice to obtain a good concentration (see SESSION 1: B.2). Gram stain and examine under the microscope as in session one. IMAGES: 10X mag 40X mag 60X mag Oil immersion Gram stain of mixed culture S. epidermidis on M-H P. aureginosa on M-H Exercise 1 file:///C|/WINDOWS/Desktop/clown/Microb Lab Web 2001/Exercise1/exercise1b.htm (6 of 6) [8/31/2002 4:29:54 PM]
Exercise 2 Cover Exercise1 EXERCISE #2 GRAM-POSITIVE COCCI AND ANTIBIOTICS Exercise2 FIRST SESSION Exercise3 FOCI 1.Identification Streptococcus by Macroscopic,Microscopic and Metabolic Exercise4 Characteristics Exercise5 2.Antibiotic susceptibility test Exercise6 Exercise7 Identification of Bacterial Genera Clinical Lactose case studies Suggestions Lactose+ Lactose Indole Glucose+ Escherichia Enebacter Mofile Non-motie,HS- Pseudomoras Urea+ Urea Shigella Protus Salmonella alm ost always bes gins as a m rphological study of the unknown sand the clincin nta requrea detot organism is a gram-positive,nonspore forming rod,then one needs to know whether or not it is acid-fast. Motility determinations are also significant especially with the gram-negative rods.These facts along with the cultural characteristics will enable the investigator to ultimately arrive at one of the nine groups of genera.A presumptive identification of the genus may also be possible at this time especially if symptoms of the clinical infection are known.Physiological tests and/or serologies are subsequently performed to confirm the genus as well as to determine the species of the etiologic agent. A.STREPTOCOCCI file://CINDOWS/Desktop/clown/Microb Lab Web 2001/Exercise2/exercise2.htm(1 of10)[/3/0:0:02 PM]
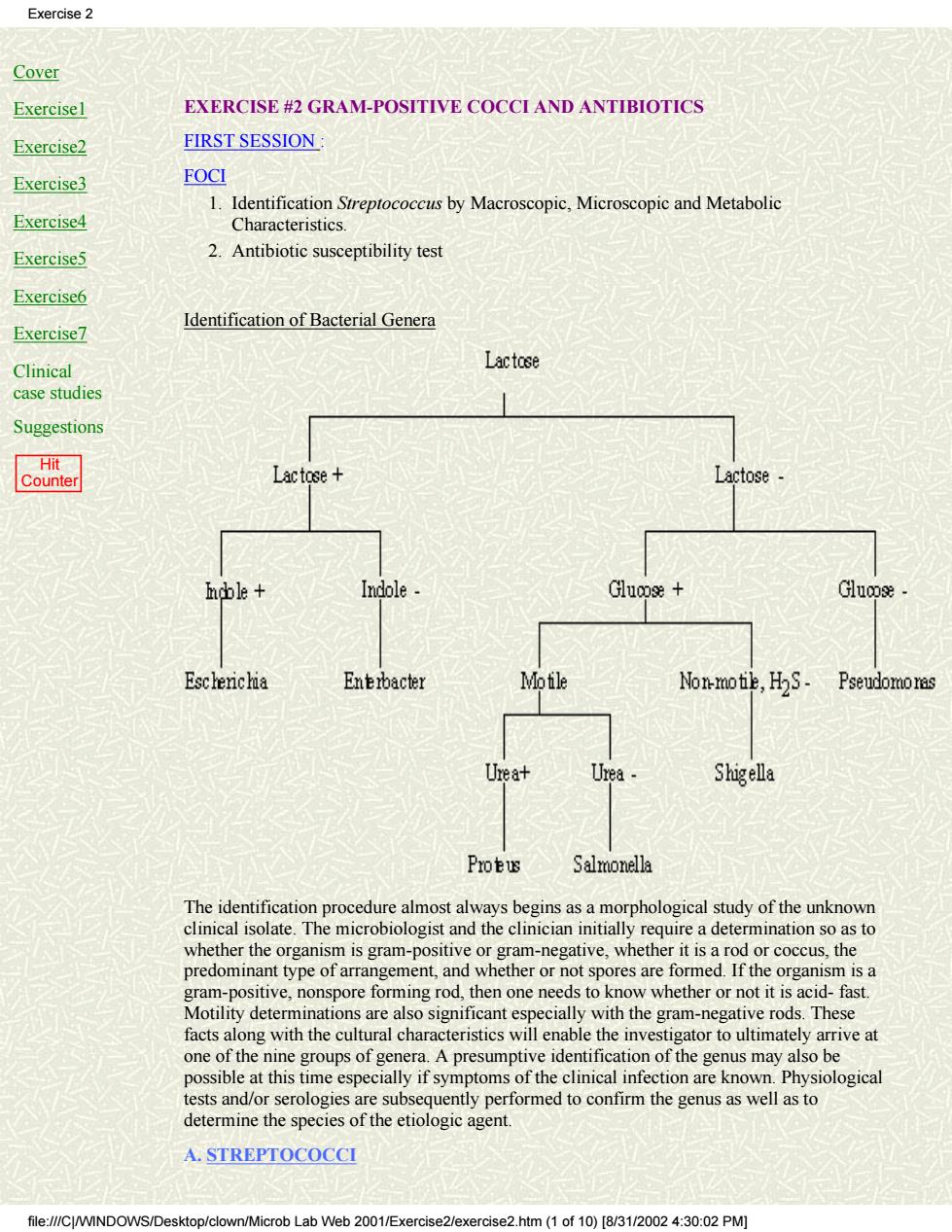
Cover Exercise1 Exercise2 Exercise3 Exercise4 Exercise5 Exercise6 Exercise7 Clinical case studies Suggestions Hit Counter EXERCISE #2 GRAM-POSITIVE COCCI AND ANTIBIOTICS FIRST SESSION : FOCI Identification Streptococcus by Macroscopic, Microscopic and Metabolic Characteristics. 1. 2. Antibiotic susceptibility test Identification of Bacterial Genera The identification procedure almost always begins as a morphological study of the unknown clinical isolate. The microbiologist and the clinician initially require a determination so as to whether the organism is gram-positive or gram-negative, whether it is a rod or coccus, the predominant type of arrangement, and whether or not spores are formed. If the organism is a gram-positive, nonspore forming rod, then one needs to know whether or not it is acid- fast. Motility determinations are also significant especially with the gram-negative rods. These facts along with the cultural characteristics will enable the investigator to ultimately arrive at one of the nine groups of genera. A presumptive identification of the genus may also be possible at this time especially if symptoms of the clinical infection are known. Physiological tests and/or serologies are subsequently performed to confirm the genus as well as to determine the species of the etiologic agent. A. STREPTOCOCCI Exercise 2 file:///C|/WINDOWS/Desktop/clown/Microb Lab Web 2001/Exercise2/exercise2.htm (1 of 10) [8/31/2002 4:30:02 PM]
Exercise 2 Sreptococci are gram-positive cocci which typically occur in chains,clusters,and pairs. The that fo in nt hac the mout orm the dom ial flora of gastrointestinal tract Streptococcus pyogenes (Lancefield's GroupA,beta-hemolytic streptococci)is the most reknown pathogen in this genus.It causes infections such as acute pharyngitis(strep sore throat),impetigo,post-operative wound infections,cellulitis,erysipelas,post-streptococcal glomerulonephritis,and acute rheumatic fever.Asymptomatic colonization of S.pyogenes in the pharynx and on skin surfaces as well as anal carriage is not uncommon and may serve as a source of infection. Streptococcus agalactiae(Lancefield's Group B,beta-hemolytic streptococci)can be vered from the g nital and intestinal t arently healthy adults and children.It is primarily i ated i natal infectio s pn ia and/or he it ha Enterococcus faecalis(Lancefield's Group D,nonhemolytic streptococci)is normally found in the intestinal tract along with other enterococci(E.faecium and E.durans).It causes infections such as subacute bacterial endocarditis(20%),urinary tract infections(10%), wound infections,and some other opportunistic infections.The resistance of enterococcal species to penicillin is an important fact to remember in treating patients infected with these streptococci. eumoniae can be isolated from the pharynx of 30-70%of apparently healthy rimarily causes a bacterial r monia ially in the debilitated or compr atients with conjunctivitis meningitis,otitis,pericarditis,empyemaendocarditis,and septicemia Viridans streptococci includes about 10 species(S.mutans.S.sanguis.S.salivarius)which are normally found in the mouth and pharynx.These streptococci are usually alpha or non-hemolytic on blood agar and cause about 50-70%of all subacute bacterial endocarditis They have also been implicated in causing dental caries,bacteremia,and sepsis. Blood agar plate cultures of each of the following microorganisms will be available for student examination a Streptococcus(Group A Streptococci) b.Streptococcus agalactiae (Group B Streptococci) c.Streptococcus pneumoniae(Pneumococci) d.Enterococcus faecalis(Group D Streptococci) >>> Each student should use one of these cultures to perform the following tests. 1.Describe the cultural characteristics of the various streptococci on blood agar medium Note the type.size.and color of the colonies and describe the various types of hemolysis observed with these microorganisms. Streptococcus pyogenes Streptococcus agalactiae Streptococcus pneumoniae Enterococcus faecalis file://CWIND n/Microb Lab Web 2001/Exercise2/exercise2.htm(2 of 10)[8/31/2002 4:30:02 PM]
Streptococci are gram-positive cocci which typically occur in chains, clusters, and pairs. There are many members of the genus Streptococcus that form the dominant bacterial flora of the mouth and the pharynx. Some streptococcal species are normally found in the gastrointestinal tract. Streptococcus pyogenes (Lancefield's GroupA, beta-hemolytic streptococci) is the most reknown pathogen in this genus. It causes infections such as acute pharyngitis (strep sore throat), impetigo, post-operative wound infections, cellulitis, erysipelas, post-streptococcal glomerulonephritis, and acute rheumatic fever. Asymptomatic colonization of S. pyogenes in the pharynx and on skin surfaces as well as anal carriage is not uncommon and may serve as a source of infection. Streptococcus agalactiae (Lancefield's Group B, beta-hemolytic streptococci) can be recovered from the genital and intestinal tract of apparently healthy adults and children. It is primarily implicated in causing neonatal infections such as pneumonia, septicemia and/or meningitis. Nevertheless, it has been isolated from patients with urinary tract infections, wound infections and otitis media. Enterococcus faecalis (Lancefield's Group D, nonhemolytic streptococci) is normally found in the intestinal tract along with other enterococci (E. faecium and E. durans). It causes infections such as subacute bacterial endocarditis (20%), urinary tract infections (10%), wound infections, and some other opportunistic infections. The resistance of enterococcal species to penicillin is an important fact to remember in treating patients infected with these streptococci. Streptococcus pneumoniae can be isolated from the pharynx of 30-70% of apparently healthy individuals. It primarily causes a bacterial pneumonia especially in the debilitated or compromised patient. This diplococcus has also been isolated in patients with conjunctivitis, meningitis, otitis, pericarditis, empyema, endocarditis, and septicemia. Viridans streptococci includes about 10 species (S. mutans, S. sanguis, S. salivarius) which are normally found in the mouth and pharynx. These streptococci are usually alpha or non-hemolytic on blood agar and cause about 50-70% of all subacute bacterial endocarditis. They have also been implicated in causing dental caries, bacteremia, and sepsis. Blood agar plate cultures of each of the following microorganisms will be available for student examination: a. Streptococcus (Group A Streptococci) b. Streptococcus agalactiae (Group B Streptococci) c. Streptococcus pneumoniae (Pneumococci) d. Enterococcus faecalis (Group D Streptococci) >>>>> Each student should use one of these cultures to perform the following tests. 1. Describe the cultural characteristics of the various streptococci on blood agar medium. Note the type, size, and color of the colonies and describe the various types of hemolysis observed with these microorganisms. Streptococcus pyogenes Streptococcus agalactiae Streptococcus pneumoniae Enterococcus faecalis Exercise 2 file:///C|/WINDOWS/Desktop/clown/Microb Lab Web 2001/Exercise2/exercise2.htm (2 of 10) [8/31/2002 4:30:02 PM]
Exercise 2 1.Examine bacteria microscopically by preparing a gram stain. Streptococcus pyogenes Streptococcus agalactiae Streptococcus pneumoniae Enterococcus faecalis 2.Catalase Test--Perform the slide test by emulsifying some visible growth material in a drop of hydrogen peroxide and note that all streptococci are catalase-negative(no rapid ebullition). 3.Rapid Enterococcus Identification--The bile esculin(BE)test is the most accurate way for identifying Group D streptococci because they are all BE-positive and will cause a blackening of the agar medium after overnight incubation.All other streptococci are negative for this reaction.An enterococcus/Group A screen will be available for the rapid identification of Enterococcus faecalis from other streptococci.This specific medium contains esculin and also PYR(pyroglutamylbeta-naphthylamide)which will differentiate enterococci from other Group D streptococci. a)Using a sterile lo obtain a visible,he avy ino mn an stab into the medium in an area near one side next to the glass.Incubate the tube at 35C for 30 minutes to 4 hours b)The esculin hydrolysis usually occurs in 30 minutes with a heavy inoculum and is indicated by development of a dark brown color.The PYR reaction is detected by adding 2 drops of the PYR reagent and observing a cherry red color within 2 minutes.No color change,light orange or light pink-orange is considered negative. Positive and Negative Reactions of BE-PYR strep om other het tc streptoc cci by eaction The usually requires the inoculation of bile esculin agar and tube of broth containing6.5%NaCl d)After overnight incubation,the black discoloration of bile esculin identifies Group D streptococci(E.faecalis,S.bovis,etc.)and growth in the presence of 6.5%NaCl (salt tolerance test)differentiates enterococci which are salt tolerant from other Group D streptococci(S.bovis)which will not grow in this broth. Group A Groups GrOUD D GrOuD D B.CF.G Enterococcus Non-Enterococcus Esculin 十 十 PYR x 、 5.Rapid Streptococeal Grouping Most streptococcal species possess group specific antigens which are usually carbohydrate structural components of the cell wall.These antigens can be extracted and identified by homologous antisera,and the bacterium can be assigned to one of the various Lancefield groups.The principal use of the test is to rapidly identify strepto reported with one hour extraction from r wound swabs). Extraction and Test Procedure: a.To a small glass tube,2 drops of reagent I and 2 drops of reagent 2 are added to generate file://CJ/WINDOWS/Desktop/clown/Microb Lab Web 2001/Exercise2/exercise2.htm (3 of 10)[8/31/0024:30:02 PM]
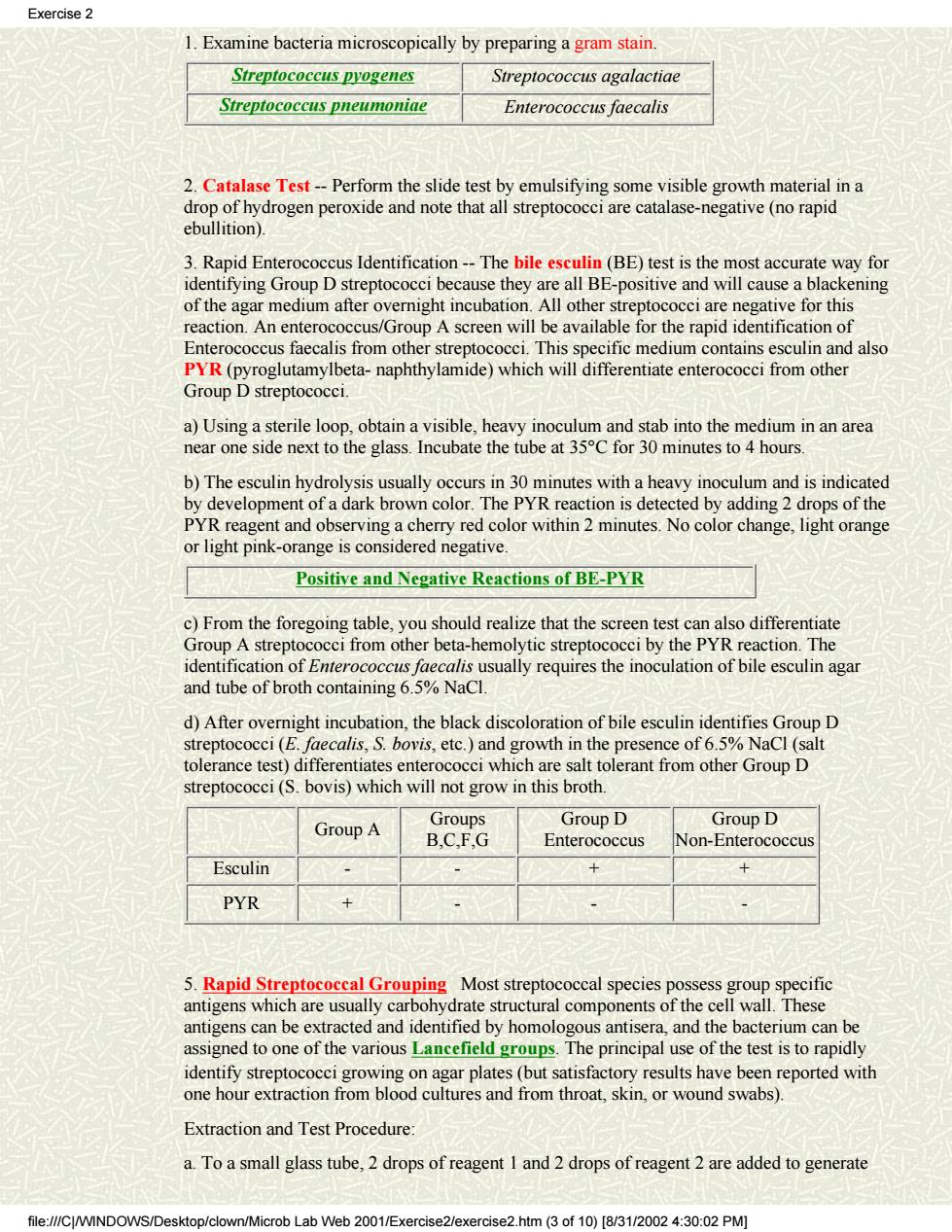
1. Examine bacteria microscopically by preparing a gram stain. Streptococcus pyogenes Streptococcus agalactiae Streptococcus pneumoniae Enterococcus faecalis 2. Catalase Test -- Perform the slide test by emulsifying some visible growth material in a drop of hydrogen peroxide and note that all streptococci are catalase-negative (no rapid ebullition). 3. Rapid Enterococcus Identification -- The bile esculin (BE) test is the most accurate way for identifying Group D streptococci because they are all BE-positive and will cause a blackening of the agar medium after overnight incubation. All other streptococci are negative for this reaction. An enterococcus/Group A screen will be available for the rapid identification of Enterococcus faecalis from other streptococci. This specific medium contains esculin and also PYR (pyroglutamylbeta- naphthylamide) which will differentiate enterococci from other Group D streptococci. a) Using a sterile loop, obtain a visible, heavy inoculum and stab into the medium in an area near one side next to the glass. Incubate the tube at 35°C for 30 minutes to 4 hours. b) The esculin hydrolysis usually occurs in 30 minutes with a heavy inoculum and is indicated by development of a dark brown color. The PYR reaction is detected by adding 2 drops of the PYR reagent and observing a cherry red color within 2 minutes. No color change, light orange or light pink-orange is considered negative. Positive and Negative Reactions of BE-PYR c) From the foregoing table, you should realize that the screen test can also differentiate Group A streptococci from other beta-hemolytic streptococci by the PYR reaction. The identification of Enterococcus faecalis usually requires the inoculation of bile esculin agar and tube of broth containing 6.5% NaCl. d) After overnight incubation, the black discoloration of bile esculin identifies Group D streptococci (E. faecalis, S. bovis, etc.) and growth in the presence of 6.5% NaCl (salt tolerance test) differentiates enterococci which are salt tolerant from other Group D streptococci (S. bovis) which will not grow in this broth. Group A Groups B,C,F,G Group D Enterococcus Group D Non-Enterococcus Esculin - - + + PYR + - - - 5. Rapid Streptococcal Grouping Most streptococcal species possess group specific antigens which are usually carbohydrate structural components of the cell wall. These antigens can be extracted and identified by homologous antisera, and the bacterium can be assigned to one of the various Lancefield groups. The principal use of the test is to rapidly identify streptococci growing on agar plates (but satisfactory results have been reported with one hour extraction from blood cultures and from throat, skin, or wound swabs). Extraction and Test Procedure: a. To a small glass tube, 2 drops of reagent 1 and 2 drops of reagent 2 are added to generate Exercise 2 file:///C|/WINDOWS/Desktop/clown/Microb Lab Web 2001/Exercise2/exercise2.htm (3 of 10) [8/31/2002 4:30:02 PM]