新生儿呼吸困难
新生儿呼吸困难
位31岁孕妇,G2P1,怀孕已29周,孕期检 查正常,今天上午感觉开始宫缩,住院检查,宫 口开3cm,约每20分钟一次宫缩,已破膜,并有 低热,37.90℃。 产科医师请新生儿科医师会诊,这位孕妇可能 要早产,怎么处理? 各位医师有什么建议?
一位31岁孕妇,G2P1,怀孕已29周,孕期检 查正常,今天上午感觉开始宫缩,住院检查,宫 口开3cm,约每20分钟一次宫缩,已破膜,并有 低热, 37.9OC。 产科医师请新生儿科医师会诊,这位孕妇可能 要早产,怎么处理? 各位医师有什么建议?
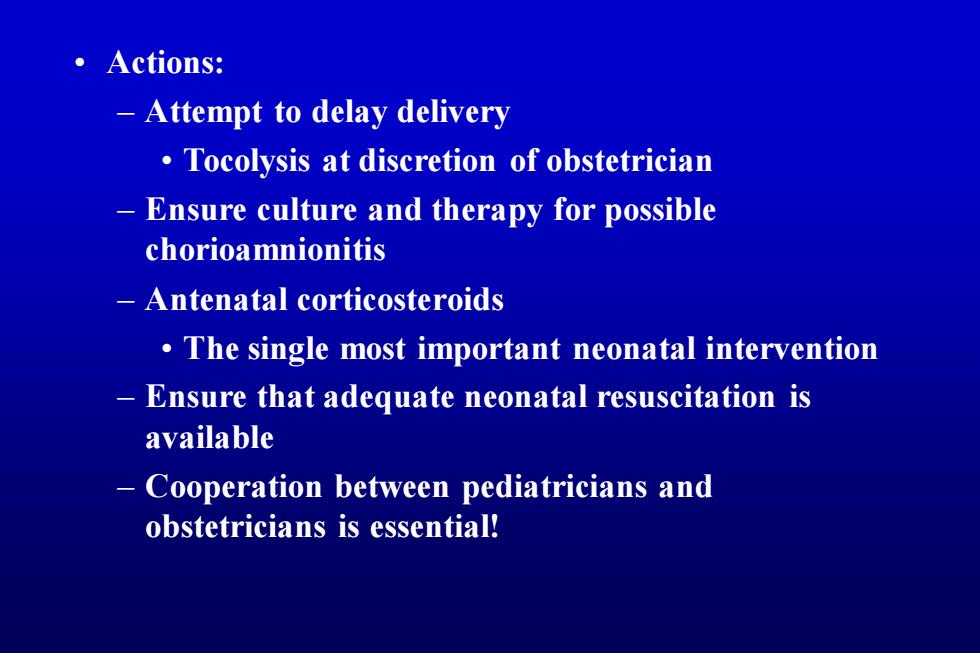
·Actions: Attempt to delay delivery Tocolysis at discretion of obstetrician Ensure culture and therapy for possible chorioamnionitis Antenatal corticosteroids The single most important neonatal intervention Ensure that adequate neonatal resuscitation is available Cooperation between pediatricians and obstetricians is essential!
• Actions: – Attempt to delay delivery • Tocolysis at discretion of obstetrician – Ensure culture and therapy for possible chorioamnionitis – Antenatal corticosteroids • The single most important neonatal intervention – Ensure that adequate neonatal resuscitation is available – Cooperation between pediatricians and obstetricians is essential!
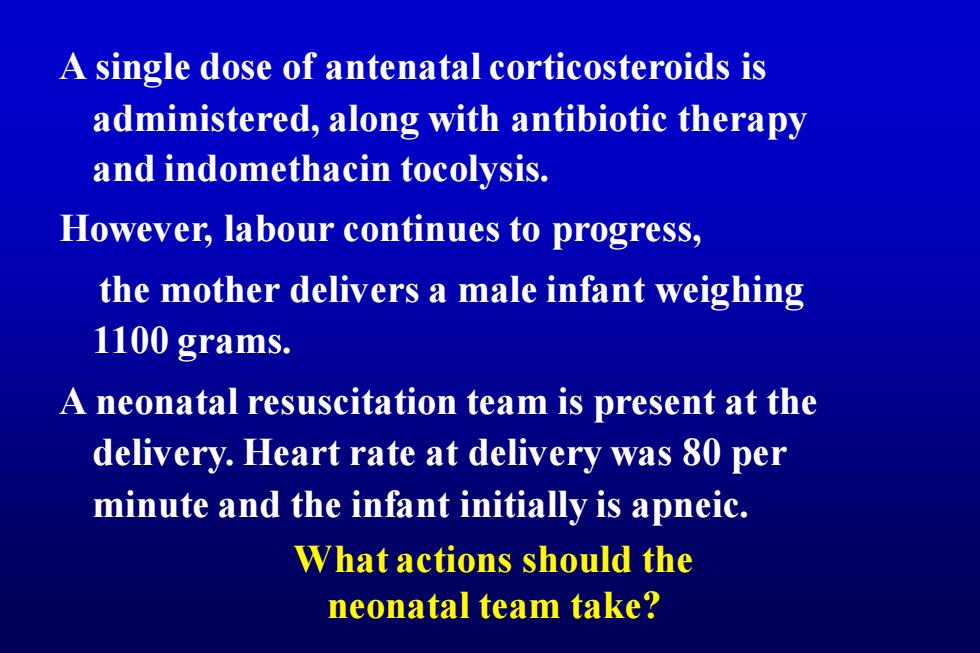
A single dose of antenatal corticosteroids is administered,along with antibiotic therapy and indomethacin tocolysis. However,labour continues to progress, the mother delivers a male infant weighing 1100 grams. A neonatal resuscitation team is present at the delivery.Heart rate at delivery was 80 per minute and the infant initially is apneic. What actions should the neonatal team take?
A single dose of antenatal corticosteroids is administered, along with antibiotic therapy and indomethacin tocolysis. However, labour continues to progress, the mother delivers a male infant weighing 1100 grams. A neonatal resuscitation team is present at the delivery. Heart rate at delivery was 80 per minute and the infant initially is apneic. What actions should the neonatal team take?
。Actions: Suction,drying,stimulation. If apneic,bag mask ventilation If no response,intubation (3.0 ETT) -Administer oxygen If persistently bradycardic despite adequate ventilation -cardiac compressions If no response,epinephrine per ETT Immediate,skilled resuscitation is essential to optimize outcomes
• Actions: – Suction, drying, stimulation. – If apneic, bag mask ventilation • If no response, intubation (3.0 ETT) – Administer oxygen – If persistently bradycardic despite adequate ventilation → cardiac compressions • If no response, epinephrine per ETT – Immediate, skilled resuscitation is essential to optimize outcomes