
重庆医科大学儿科学教案讲课题目:Neonatal Jaundice新生儿黄痘教师:余加林授课题目TEACHINGTOPICNeonatal Jaundice新生儿黄痘第几次课TIMES3r教学方法METHODSClass teaching教学对象OBJECTIVESeven years students学时:TIME40×2 minutes教学目标PURPOSE1.master differentiate diagnosisof physiological jaundice andpathological jaundicehe clinical featuofneonatalhemolyticsorders,neonatalnatehepatitis and biliary atresizknow the features of bilirubin metabolism in neonatesknowtheriskfactors andprophylactic approaches ofkernicterusfamiliar withtheclinicalfeaturesof common disorderscausing2pathological jaundices教学重点和难点1.the features of bilirubinmetabolism in nconatesPURPOSEIDIFFICULTIES2.thefactors aggravating neonatal jaundice3. the maternal and newborn blood types related to isoimmunization教学内容的深化与拓宽Introduce of factors relating to kernicterus.Thedevelopments教学要求的英语单词Jaundice, hyperbilirubinemia, Physiological phenomenon, Pathologic signEnglish requirementsUnconjugated bilirubin, basal ganglia, kernicterus.liver cirrhosis,biliaryatresia, Diagnostic Criteria, TORCHS: toxoplasma, protozoom, rubella,cytomegalovirus,herpes,HIV,syphilis,Hemolytic disorders,ABincompatibility实践性教学安排On teachinghouroelinicalworkshoClinical study教材及参考资料沈晓明,王卫平。儿科学,北京:人民卫生出版社,2008TEXTUSEDI杨锡强,易著文儿科学,北京:人民卫生出版社,2008BOOKREFERENCES3TaeuschHW,BllardRAGleasonAEsevierSaundersAverysdiasthwnditn0教具 TEACHING AIDSPP教学程序Procedures详细见讲稿主要内容及安排(教学内容详细安排、教学方法的运用、师生活动设计、及时间分配):
重庆医科大学儿科学教案 讲课题目:Neonatal Jaundice 新生儿黄疸 教师: 余加林 授课题目 TEACHING TOPIC Neonatal Jaundice 新生儿黄疸 第几次课 TIMES 3 rd 教学方法 METHODS Class teaching 教学对象 OBJECTIVE Seven years students 学时: TIME 40×2 minutes 教学目标 PURPOSE 1. master differentiate diagnosis of physiological jaundice and pathological jaundice 2. mater the clinical features of neonatal hemolytic disorders, neonatal hepatitis and biliary atresia 3. know the features of bilirubin metabolism in neonates 4. know the risk factors and prophylactic approaches of kernicterus 5. familiar with the clinical features of common disorders causing pathological jaundices 教学重点和难点 PURPOSE/ DIFFICULTIES 1. the features of bilirubin metabolism in neonates 2. the factors aggravating neonatal jaundice 3. the maternal and newborn blood types related to isoimmunization 教学内容的深化与拓宽 The developments Introduce of factors relating to kernicterus. 教学要求的英语单词 English requirements Jaundice,hyperbilirubinemia,Physiological phenomenon,Pathologic sign, Unconjugated bilirubin,basal ganglia, kernicterus.liver cirrhosis, biliary atresia,Diagnostic Criteria,TORCHS: toxoplasma,protozoom,rubella, cytomegalovirus , herpes, HIV , syphilis, Hemolytic disorders, ABO incompatibility 实践性教学安排 Clinical study One teaching hour of clinical workshop. 教材及参考资料 TEXT BOOK USED/ REFERENCES 1. 沈晓明,王卫平. 儿科学. 北京: 人民卫生出版社, 2008 2. 杨锡强,易著文. 儿科学. 北京: 人民卫生出版社, 2008 3.Taeusch HW, Ballard RA, Gleason CA. Elsevier Saunders: Avery’s diseases of the newborn, 8th edition, 2005 教具 TEACHING AIDS PPT 教学程序 Procedures (教学内容详细安排、教学方法的运用、师生活动设计、及时间分配): 详细见讲稿主要内容及安排

讲稿主要内容及安排备注(授课形时间安式)排题目(分钟)Neonatal Jaundice[概述] NTRODUCTIONNeonatal jaundice also as hyperbilirubinemia, Within 1 week of age , incident of visiblyjaundice :60% infull-term infants80% inpreterm infants5'Class teachingSignificance of Jaundice in newborn :Physiological phermenor2. Pathologic signIt may be a sign of another disorder ,e.g infection. Unconjugated bilirubin can bedositedithe baaruyithe bsagangliaaungkeuMaydevelop intoliver cirhossifbiliay atresianotperformhepatoportoenterostomy in time【新生儿胆红素代谢特点】Summary of neonatal bilirubin metabolism1. Bilirubin loadClass teaching152Abuminnotenoughctivetanspo3.Immaturityof liver enzymes4.Treabsorptionofbilirubinfrom gutNeonatal infants are easy tohappen jaundice and become pathologicjaundiceClass teaching 10°[诊断标准]】 DiagnosticCriteria
讲稿主要内容及安排 题目 备注(授课形 式) 时间安 排 (分 钟) Neonatal Jaundice Class teaching 5’ [概述] INTRODUCTION Neonatal jaundice also as hyperbilirubinemia, Within 1 week of age,incident of visibly jaundice:60% in full-term infants,80% in preterm infants. Significance of Jaundice in newborn: 1.Physiological phenomenon 2.Pathologic sign: It may be a sign of another disorder ,e.g. infection. Unconjugated bilirubin can be deposited in the brain, particularly in the basal ganglia, causing kernicterus. May develop into liver cirrhosis if biliary atresia not perform hepatoportoenterostomy in time. [新生儿胆红素代谢特点] Summary of neonatal bilirubin metabolism Class teaching 15’ 1. ↑Bilirubin load 2. Albumin not enough: Defective transport 3. Immaturity of liver enzymes 4. ↑reabsorption of bilirubin from gut Neonatal infants are easy to happen jaundice and become pathologic jaundice. [诊断标准] Diagnostic Criteria Class teaching 10’
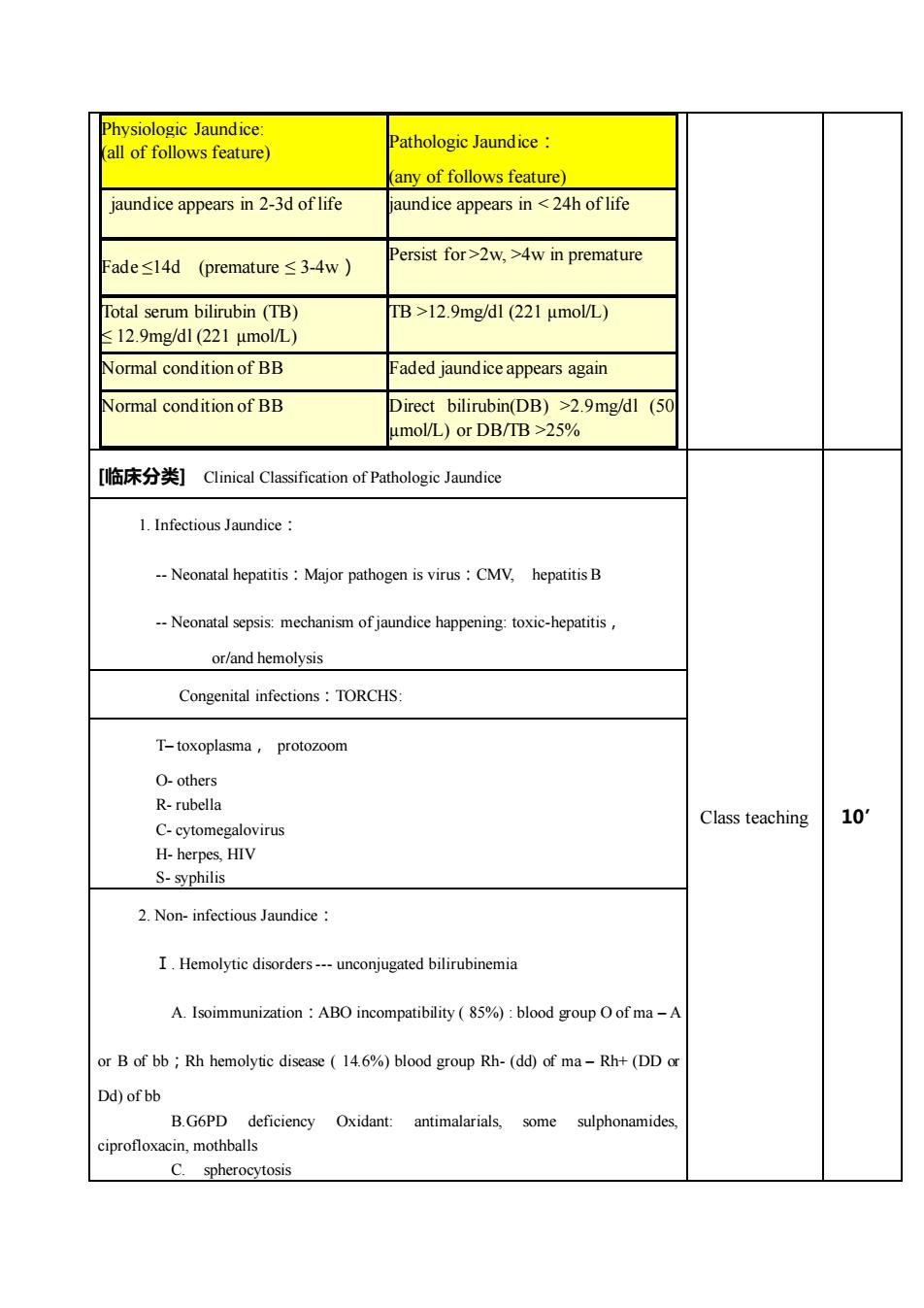
Physiologic JaundicePathologic Jaundice :alloffollowsfeature)(any offollows feature)jaundice appears in2-3d oflifejaundice appears in<24h of lifePersist for>2w,>4w in prematureFade≤14d (premature≤3-4w)Total serum bilirubin (TB)TB>12.9mg/dl (221 μmol/L)12.9mg/dl (221 μmol/L)Normal cond ition of BBFaded jaundiceappears againDirect bilirubin(DB) >2.9mg/dl (50Normal condition of BBumol/L)orDB/IB>25%[临床分类] Clinical Classification of Pathologic JaundiceI. Infectious Jaundice : Neonatal hepatitis : Major pathogen is virus : CMV, hepatitis B-- Neonatal sepsis: mechanism of jaundice happening: toxic-hepatitis ,or/and hemolysisCongenital infections : TORCHS:T-toxoplasma, protozoomO- othersR- rubella10'Class teachingC- cytomegalovirusH- herpes, HIVS- syphilis2. Non- infectious Jaundice :I.Hemolytic disorders--- unconjugated bilirubinemiaA. Isoimmunization : ABO incompatibility ( 85%) : blood group O of ma -Aor B of bb ; Rh hemolytic disease (14.6%) blood group Rh-(dd) of ma -Rh+ (DD oDd) of bBGPD deficieney Oxidant:antimalarials,some sulphonamidesciprofloxacin, mothballsC.spherocytosis
Physiologic Jaundice: (all of follows feature) Pathologic Jaundice: (any of follows feature) jaundice appears in 2-3d of life jaundice appears in < 24h of life Fade ≤14d (premature ≤ 3-4w) Persist for >2w, >4w in premature Total serum bilirubin (TB) ≤ 12.9mg/dl (221 µmol/L) TB >12.9mg/dl (221 µmol/L) Normal condition of BB Faded jaundice appears again Normal condition of BB Direct bilirubin(DB) >2.9mg/dl (50 µmol/L) or DB/TB >25% [临床分类] Clinical Classification of Pathologic Jaundice Class teaching 10’ 1. Infectious Jaundice: - Neonatal hepatitis:Major pathogen is virus:CMV, hepatitis B - Neonatal sepsis: mechanism of jaundice happening: toxic-hepatitis, or/and hemolysis Congenital infections:TORCHS: T– toxoplasma, protozoom O- others R- rubella C- cytomegalovirus H- herpes, HIV S- syphilis 2. Non- infectious Jaundice: Ⅰ. Hemolytic disorders - unconjugated bilirubinemia A. Isoimmunization:ABO incompatibility ( 85%) : blood group O of ma – A or B of bb;Rh hemolytic disease ( 14.6%) blood group Rh- (dd) of ma – Rh+ (DD or Dd) of bb B.G6PD deficiency Oxidant: antimalarials, some sulphonamides, ciprofloxacin, mothballs C. spherocytosis
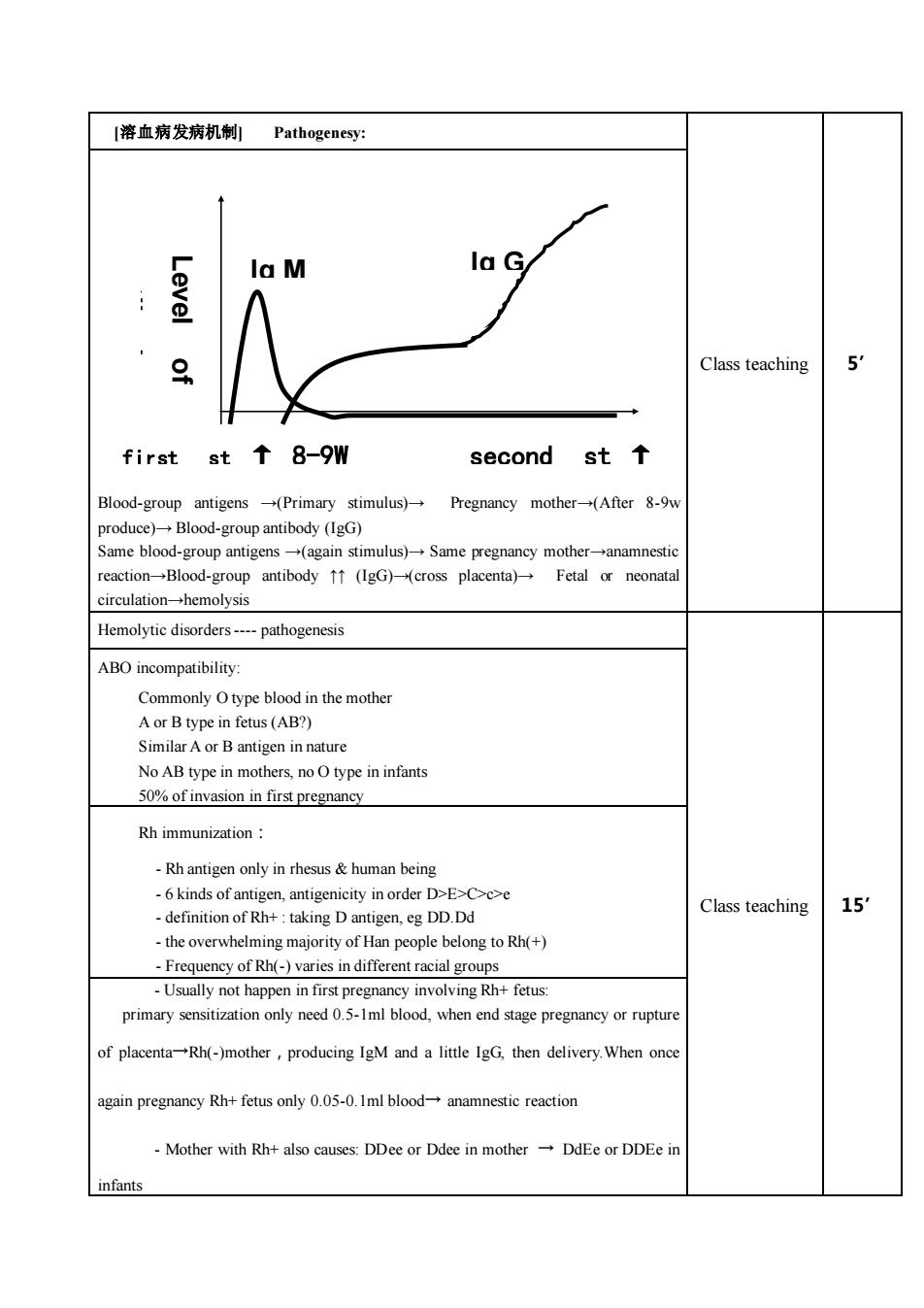
[溶血病发病机制]Pathogenesy:lala M20 Class teaching 5O8-9Wsecondst ↑firstst(Primary stimulus)-Pregnancy mother-(After 8-9wBlood-groupantigensproduce) Blood-group antibody (IgG)Same blood-group antigens (again stimulus) Same pregnancy mother-anamnesticreaction-→Blood-group antibody ↑↑ (IgG)(cross placenta)Fetal or neonatalcirculation-hemolysisHemolytie disordes--- athogenesisABO incompatibility:Commonly Otype blood in the motheA or B type in fetus (AB?)Similar A or B antigen in natureNo AB type in mothes.noOtypeininfant50%of invasion in first pregnancyRh immunization-Rh antigen only in rhesus & human being-6 kinds of antigen, antigenicity in order D>E>C>c>e15'Class teaching- definition of Rh+ taking D antigen, eg DD.Ddthe overwhelming majority of Han people belong to Rh(+)- Frequency of Rh(-) varies in different racial groups-Usually not happen in first pregnancy involving Rh+ fetus:primary sensitization only need 0.5-1ml blood, when end stage pregnancy or ruptureof placenta-Rh(-)mother ,producing IgM and a little IgG, then delivery.When onceagain pregnancy Rh+fetus only 0.05-0.1ml blood anamnestic reactionMother with Rh+ also causes: DDee or Ddee in mothe+DdEeorDDEe ilinfants
[溶血病发病机制] Pathogenesy: Class teaching 5’ Blood-group antigens →(Primary stimulus)→ Pregnancy mother→(After 8-9w produce)→ Blood-group antibody (IgG) Same blood-group antigens →(again stimulus)→ Same pregnancy mother→anamnestic reaction→Blood-group antibody ↑↑ (IgG)→(cross placenta)→ Fetal or neonatal circulation→hemolysis Hemolytic disorders - pathogenesis Class teaching 15’ ABO incompatibility: Commonly O type blood in the mother A or B type in fetus (AB?) Similar A or B antigen in nature No AB type in mothers, no O type in infants 50% of invasion in first pregnancy Rh immunization: - Rh antigen only in rhesus & human being - 6 kinds of antigen, antigenicity in order D>E>C>c>e - definition of Rh+ : taking D antigen, eg DD.Dd - the overwhelming majority of Han people belong to Rh(+) - Frequency of Rh(-) varies in different racial groups - Usually not happen in first pregnancy involving Rh+ fetus: primary sensitization only need 0.5-1ml blood, when end stage pregnancy or rupture of placenta→Rh(-)mother,producing IgM and a little IgG, then delivery.When once again pregnancy Rh+ fetus only 0.05-0.1ml blood→ anamnestic reaction - Mother with Rh+ also causes: DDee or Ddee in mother → DdEe or DDEe in infants first st ↑ 8-9W second st ↑ time antibody Level of Ig M Ig G
, but have exception (only1%)isuallynofirstpregnancy1.if motherbe sensitized byearlybloodtransfusior2. if mother's mother has Rh+ RBC (外祖母学说)II. Biliary Atresia-- cojugated bilirubinemia-whiteclay-colored stoolsI. Breast milk jaundice:-- 10% ofbreast-fed infants- uncojugated bilirubinemia-Ifstopfeedingbreastmilkfor3~5d,TB↓50%The most severe complication ofjaundice in newbornEncephalopathy (Kernicterus ) :-- 50% die--sequelaes:cerebralpalsy,dafssmentalretadatCritical threshold of TB : 342 μmol/L-- Usually occur during the 1-7d oflife-- Prematurrity can have low TB kernicterusrelevant factors-- concentration of bilirubin- how much unconjugated bilirubin bound to albumindegree of maturity of blood brain barrier(BBB)[治疗] Treatments1. Phototherapy : --lightswavelength 420-470nm (blue),510-530nm(green)or white未结合胆红素→水溶性异构体一排出canconvertunconjugated bilirubin intoharmless water-soluble pigment.15'Class teaching-- best widely used therapy , 12-24h workAttentions during Phototherapy-cover eyes preventing retinal damage, -- hypo-or hyperthermia--dehydration-- macular rashlarrhoea
- usually no first pregnancy happen, but have exception (only 1%) 1. if mother be sensitized by early blood transfusion 2. if mother’s mother has Rh+ RBC (外祖母学说) Ⅱ. Biliary Atresia: - cojugated bilirubinemia - white clay-colored stools Ⅲ. Breast milk jaundice: - 10% of breast-fed infants - uncojugated bilirubinemia. - If stop feeding breast milk for 3~5d, TB ↓ 50% The most severe complication of jaundice in newborn : Encephalopathy (Kernicterus): - 50% die - sequelaes: cerebral palsy, deafness, mental retardation - Critical threshold of TB:342 µmol/L - Usually occur during the 1~7d of life - Prematurrity can have low TB kernicterus relevant factors: - concentration of bilirubin - how much unconjugated bilirubin bound to albumin - degree of maturity of blood brain barrier(BBB) [治疗] Treatments Class teaching 15’ 1.Phototherapy:- lights : wavelength 420-470nm (blue) , 510-530nm (green) or white 未结合胆红素→水溶性异构体→排出 - can convert unconjugated bilirubin into harmless water-soluble pigment. - best widely used therapy,12-24h work Attentions during Phototherapy: -cover eyes preventing retinal damage, - hypo- or hyperthermia - dehydration - macular rash - diarrhoea